Multiple sclerosis
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
 |
|
|---|---|
| MRI image showing a bright spot where multiple sclerosis has damaged myelin in the brain | |
| ICD- 10 | G 35. |
| ICD- 9 | 340 |
Multiple sclerosis (abbreviated MS, also known as disseminated sclerosis) is a chronic, inflammatory disease that affects the central nervous system (CNS). MS can cause a variety of symptoms, including changes in sensation, visual problems, muscle weakness, depression, difficulties with coordination and speech, severe fatigue, and pain. Although many patients lead full and rewarding lives, MS can cause impaired mobility and disability in more severe cases.
Multiple sclerosis affects neurons, the cells of the brain and spinal cord that carry information, create thought and perception, and allow the brain to control the body. Surrounding and protecting some of these neurons is a fatty layer known as the myelin sheath, which helps neurons carry electrical signals. MS causes gradual destruction of myelin ( demyelination) and transection of neuron axons in patches throughout the brain and spinal cord. The name multiple sclerosis refers to the multiple scars (or scleroses) on the myelin sheaths. This scarring causes symptoms which vary widely depending upon which signals are interrupted. It is thought that MS results from attacks by an individual's immune system on the nervous system and is therefore categorized as an autoimmune disease.
Multiple sclerosis may take several different forms, with new symptoms occurring either in discrete attacks or slowly accruing over time. Between attacks, symptoms may resolve completely, but permanent neurologic problems often persist. Although much is known about how MS causes damage, its exact cause remains unknown. MS currently does not have a cure, though several treatments are available which may slow the appearance of new symptoms. MS primarily affects adults, with an age of onset typically between 20 and 40 years, and is more common in women than in men.
Common symptoms
Individuals with multiple sclerosis may experience a wide variety of symptoms. The initial attacks are often transient, mild (or asymptomatic), and self-limited. They often do not prompt a health care visit and sometimes are only identified in retrospect once the diagnosis has been made based on further attacks. The most common initial symptoms reported are: changes in sensation in the arms, legs or face (33%), complete or partial vision loss ( optic neuritis) (16%), weakness (13%), double vision (7%), unsteadiness when walking (5%), and balance problems (3%). Fifteen percent of individuals have multiple symptoms when they first seek medical attention. Most people find their initial MS symptoms occur over a period of hours to weeks. For some people the initial MS attack is preceded by infection, trauma or strenuous physical effort.
Other symptoms and physical findings common in multiple sclerosis are flickering eye movements ( nystagmus), speech difficulties, tremor, clumsiness of the hands, abnormal muscle spasms, and bladder and bowel difficulties. Cognitive impairments are also common, such as difficulty performing multiple tasks at once, difficulty following detailed instructions, loss of short term memory, emotional instability, and fatigue. Emotional symptoms are common and can be the normal response to having a debilitating disease or the result of damage to the nerves that generate and control emotions. The most common condition, clinical depression, is a product of both causes. Feelings such as anger, anxiety, frustration, and hopelessness are also common, and suicide is a very real threat. People with MS may also experience a range of acute and chronic pain syndromes.
Three clinical entities warrant further discussion because affected individuals are often eventually diagnosed with MS. (However, MS is only one of several potential causes for these entities.)
- Optic neuritis
- Individuals typically experience rapid onset of pain in one eye, followed by blurry vision in part or all of the visual field of that eye. This is a result of involvement of the optic nerve by MS. Only 10% to 50% of patients (depending on the population studied) with optic neuritis go on to develop MS. The blurred vision usually resolves within six months, but individuals are often left with less vivid colour vision (especially red) in the affected eye.
- Internuclear ophthalmoplegia
- Individuals usually notice binocular diplopia (double vision with both eyes open) when looking to one side. Internuclear ophthalmoplegia occurs when MS affects a part of the brain stem called the medial longitudinal fasciculus, which is responsible for communication between the two eyes. This results in the failure of the medial rectus muscle to contract appropriately, so that the eyes do not move equally (called disconjugate gaze).
- Transverse myelitis
- Individuals typically develop rapid onset of numbness, weakness, bowel or bladder dysfunction, and/or loss of muscle function, typically in the lower half of the body. This is the result of MS attacking the spinal cord. As many as 80% of individuals with transverse myelitis are left with lasting disabilities, even though there is usually some improvement during the first two years. MS can devastate lives or it can be a life changing experience.
Diagnosis
Multiple sclerosis is difficult to diagnose in its early stages. In fact, definite diagnosis of MS cannot be made until there is evidence of at least two anatomically separate demyelinating events occurring at least thirty days apart. The McDonald criteria represent international efforts to standardize the diagnosis of MS using clinical data, laboratory data, and radiologic data.
- Clinical data alone may be sufficient for a diagnosis of MS. If an individual has suffered two separate episodes of neurologic symptoms characteristic of MS, and the individual also has consistent abnormalities on physical examination, a diagnosis of MS can be made with no further testing. Since some people with MS seek medical attention after only one attack, other testing may hasten the diagnosis and allow earlier initiation of therapy.
- Magnetic resonance imaging (MRI) of the brain and spine is often used to evaluate individuals with suspected MS. MRI shows areas of demyelination as bright lesions on T2-weighted images or FLAIR (fluid attenuated inversion recovery) sequences. Gadolinium contrast is used to demonstrate active plaques on T1-weighted images. Because MRI can reveal lesions which occurred previously but produced no clinical symptoms, it can provide the evidence of chronicity needed for a definite diagnosis of MS.
- Testing of cerebrospinal fluid (CSF) can provide evidence of chronic inflammation of the central nervous system. The CSF is tested for oligoclonal bands, which are immunoglobulins found in 85% to 95% of people with definite MS (but also found in people with other diseases). Combined with MRI and clinical data, the presence of oligoclonal bands can help make a definite diagnosis of MS. Lumbar puncture is the procedure used to collect a sample of CSF.
- The brain of a person with MS often responds less actively to stimulation of the optic nerve and sensory nerves. These brain responses can be examined using Visual evoked potentials (VEPs) and somatosensory evoked potentials (SEPs). Decreased activity on either test can reveal demyelination which may be otherwise asymptomatic. Along with other data, these exams can help find the widespread nerve involvement required for a definite diagnosis of MS.
Another test which may become important in the future is measurement of antibodies against myelin proteins such as myelin oligodendrocyte glycoprotein (MOG) and myelin basic protein (MBP). As of 2005, however, there is no established role for these tests in diagnosing MS.
The signs and symptoms of MS can be similar to other medical problems, such as stroke, brain inflammation, infections such as Lyme disease (which can produce identical MRI lesions and CSF abnormalities), tumors, and other autoimmune problems, such as lupus. Additional testing may be needed to help distinguish MS from these other problems.
Disease course and clinical subtypes
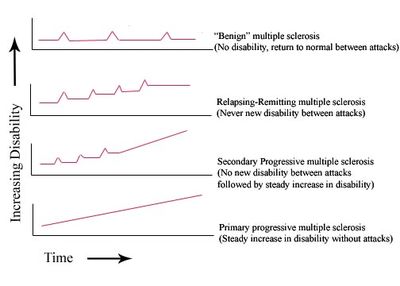
The course of MS is difficult to predict, and the disease may at times either lie dormant or progress steadily. Several subtypes, or patterns of progression, have been described. Subtypes use the past course of the disease in an attempt to predict the future course. A person diagnosed with a particular subtype may, for unclear reasons, switch from one subtype to another over time. Subtypes are important not only for prognosis but also for therapeutic decisions. In 1996 the United States National Multiple Sclerosis Society standardized the following four subtype definitions:
- Relapsing-remitting
- Relapsing-remitting describes the initial course of 85% to 90% of individuals with MS. This subtype is characterized by unpredictable attacks ( relapses) followed by periods of months to years of relative quiet ( remission) with no new signs of disease activity. Deficits suffered during the attacks may either resolve or may be permanent. When deficits always resolve between attacks, this is referred to as " benign" MS.
- Secondary progressive
- Secondary progressive describes around 80% of those with initial relapsing-remitting MS, who then begin to have neurologic decline between their acute attacks without any definite periods of remission. This decline may include new neurologic symptoms, worsening cognitive function, or other deficits. Secondary progressive is the most common type of MS and causes the greatest amount of disability.
- Primary progressive
- Primary progressive describes the approximately 10% of individuals who never have remission after their initial MS symptoms. Decline occurs continuously without clear attacks. The primary progressive subtype tends to affect people who are older at disease onset.
- Progressive relapsing
- Progressive relapsing describes those individuals who, from the onset of their MS, have a steady neurologic decline but also suffer superimposed attacks.
Factors triggering a relapse
Multiple sclerosis relapses are often unpredictable and can occur without warning with no obvious inciting factors. Some attacks, however, are preceded by common triggers. In general, relapses occur more frequently during spring and summer than during autumn and winter. Infections, such as the common cold, influenza, and gastroenteritis, increase the risk for a relapse. Emotional and physical stress may also trigger an attack, as can severe illness of any kind. Statistically, there is no good evidence that either trauma or surgery trigger relapses. People with MS can participate in sports, but they should probably avoid extremely strenuous exertion, such as marathon running. Heat can transiently increase symptoms, which is known as Uhthoff's phenomenon. This is why some people with MS avoid saunas or even hot showers. However, heat is not an established trigger of relapses.
Pregnancy can directly affect the susceptibility for relapse. The last three months of pregnancy offer a natural protection against relapses. However, during the first few months after delivery, the risk for a relapse is increased 20%–40%. Pregnancy does not seem to influence long-term disability. Children born to mothers with MS are not at increased risk for birth defects or other problems.
Many potential triggers have been examined and found not to influence relapse rates in MS. Influenza vaccination is safe, does not trigger relapses, and can therefore be recommended for people with MS. There is also no evidence that hepatitis B, varicella, tetanus, or Bacille Calmette-Guerin (BCG - immunization for tuberculosis) increases the risk for relapse. In fact, recent studies have shown that the tetanus vaccine may actually have a protective effect against the development of MS.
Pathophysiology
Although much is known about how multiple sclerosis causes damage, the reasons why multiple sclerosis occurs are not known.
How multiple sclerosis causes damage
Multiple sclerosis is a disease in which the body's immune system attacks the myelin surrounding nerve cells. Myelin is a fatty substance which covers the axons of nerve cells and is important for proper nerve conduction. A special subset of white blood cells, called T cells, plays a key role in the development of MS. Under normal circumstances, these lymphocytes can distinguish between self and non-self. However, in a person with MS, these cells recognize healthy parts of the central nervous system as foreign and attack them as if they were an invading virus.
In MS, certain T cells trigger inflammatory processes when they encounter myelin, stimulating other immune cells and soluble factors like cytokines and antibodies. Normally, there is a tight barrier between the blood and brain, called the blood-brain barrier, built up of endothelial cells lining the blood vessel walls. The inflammatory processes triggered by the T cells create leaks in the blood-brain barrier. These leaks, in turn, cause a number of other damaging effects such as swelling, activation of macrophages, and more activation of cytokines and other destructive proteins such as matrix metalloproteinases. The final result is destruction of myelin, called demyelination.
Repair processes, called remyelination, also play an important role in MS. Remyelination is one of the reasons why, especially in early phases of the disease, symptoms tend to decrease or disappear temporarily. Nevertheless, nerve damage and irreversible loss of neurons occur early in MS. Often, the brain is able to compensate for some of this damage, due to an ability called neuroplasticity. MS symptoms develop as the cumulative result of multiple lesions in the brain and spinal cord. This is why symptoms can vary greatly between different individuals, depending on where their lesions occur.
The oligodendrocytes that originally formed a myelin sheath cannot completely rebuild a destroyed myelin sheath. However, the brain can recruit stem cells, which migrate from other unknown regions of the brain, differentiate into mature oligodendrocytes, and rebuild the myelin sheath. These new myelin sheaths are often not as effective as the original ones. Repeated attacks lead to successively less effective remyelinations, until a scar-like plaque is built up around the damaged axons. Under laboratory conditions, stem cells are quite capable of differentiating and remyelinating axons; it is therefore suspected that inflammatory conditions or axonal damage somehow inhibit stem cell differentiation in the body.
Pathophysiology research
Until recently, most of the data available came from post-mortem brain samples and animal models of the disease, such as the experimental autoimmune encephalomyelitis (EAE), an autoimmune disease that rodents can develop, and which is considered a possible animal model for multiple sclerosis.
In 1998, the National Multiple Sclerosis Society and the Mayo Clinic launched " The Lesion Project" to describe MS lesions as accurately as possible and to develop an accurate model of the evolution of the disease. They have used brain biopsies apart from the post-mortem samples. Four different damage patterns have been identified in the scars of the brain tissue, but the meaning of this fact remains controversial. For some researchers it means that MS is a heterogeneous disease. Other teams maintain that the shape of the scars can change from one type to other and this could be a marker of the disease action time.
The four patterns that were identified are:
- Pattern I
- The scar presents T-cells and macrophages around blood vessels, with preservation of oligodendrocytes, but no signs of complement system activation.
- Pattern II
- The scar presents T-cells and macrophages around blood vessels, with preservation of oligodendrocytes, as before, but also signs of complement system activation can be found.
- Pattern III
- The scars are diffuse with inflammation, distal oligodendrogliopathy and microglial activation. There is also loss of myelin associated glicoprotein (MAG). The scars do not surround the blood vessels, and in fact, a rim of preserved myelin appears around the vessels. There is evidence of partial remyelinization and oligodendrocyte apoptosis.
- Pattern IV
- The scar presents sharp borders and oligodendrocyte degeneration, with a rim of normal appearing white matter. There is a lack of oligodendrocytes in the centre of the scar. There is no complement activation or MAG loss.
Why multiple sclerosis occurs
Although many risk factors for multiple sclerosis have been identified, no definitive cause has been found. MS likely occurs as a result of some combination of both environmental and genetic factors. Various theories try to combine the known data into plausible explanations. Although most accept an autoimmune explanation, several theories suggest that MS is an appropriate immune response to an underlying condition.
Environmental
The most popular hypothesis is that a viral infection or retroviral reactivation primes a susceptible immune system for an abnormal reaction later in life. On a molecular level, this might occur if there is a structural similarity between the infectious virus and some component of the central nervous system, leading to eventual confusion in the immune system.
Since MS seems to be more common in people who live farther from the equator, another theory proposes that decreased sunlight exposure and possibly decreased vitamin D production may help cause MS. This theory is bolstered by recent research into the biochemistry of vitamin D, which has shown that it is an important immune system regulator.
Other theories, noting that MS is less common in children with siblings, suggest that less exposure to illness in childhood leads to an immune system which is not primed to fight infection and is thus more likely to attack the body. One explanation for this would be an imbalance between the Th1 type of helper T-cells, which fight infection, and the Th2 type, which are more active in allergy and more likely to attack the body.
Other theories describe MS as an immune response to a chronic infection. The association of MS with the Epstein-Barr virus suggests a potential viral contribution in at least some individuals. Still others believe that MS may sometimes result from a chronic infection with spirochetal bacteria, a hypothesis supported by research in which cystic forms were isolated from the cerebrospinal fluid of all MS patients in a small study. When the cysts were cultured, propagating spirochetes emerged. Another bacterium that has been implicated in MS is Chlamydophila pneumoniae; it or its DNA has been found in the cerebrospinal fluid of MS patients by several research laboratories, with one study finding that the oligoclonal bands of 14 of the 17 MS patients studied consisted largely of antibodies to Chlamydophila antigens.
Genetic
MS is not considered a hereditary disease. However, increasing scientific evidence suggests that genetics may play a role in determining a person's susceptibility to MS. Some populations, such as the Roma, Inuit, and Bantus, never get MS. The indigenous peoples of the Americas, and Asians have very low incidence rates. It is unclear whether this is due mostly to genetic or environmental factors.
In the population at large, the chance of developing MS is less than a tenth of one percent. However, if one person in a family has MS, that person's first-degree relatives—parents, children, and siblings—have a one to three percent chance of getting the disease.
For identical twins, the likelihood that the second twin may develop MS if the first twin does is about 30%; for fraternal twins (who do not inherit identical gene pools), the likelihood is closer to that for non-twin siblings, or about 4%. The fact that the rate for identical twins both developing MS is significantly less than 100% suggests that the disease is not entirely genetically controlled. Some (but definitely not all) of this effect may be due to shared exposure to something in the environment, or to the fact that some people with MS lesions remain essentially asymptomatic throughout their lives.
Further indications that more than one gene is involved in MS susceptibility comes from studies of families in which more than one member has MS. Several research teams found that people with MS inherit certain regions on individual genes more frequently than people without MS. Of particular interest is the human leukocyte antigen (HLA) or major histocompatibility complex region on chromosome 6. HLAs are genetically determined proteins that influence the immune system.
The HLA patterns of MS patients tend to be different from those of people without the disease. Investigations in northern Europe and America have detected three HLAs that are more prevalent in people with MS than in the general population. Studies of American MS patients have shown that people with MS also tend to exhibit these HLAs in combination-that is, they have more than one of the three HLAs-more frequently than the rest of the population. Furthermore, there is evidence that different combinations of the HLAs may correspond to variations in disease severity and progression.
Studies of families with multiple cases of MS and research comparing genetic regions of humans to those of mice with EAE suggest that another area related to MS susceptibility may be located on chromosome 5. Other regions on chromosomes 2, 3, 7, 11, 17, 19, and X have also been identified as possibly containing genes involved in the development of MS.
These studies strengthen the theory that MS is the result of a number of factors rather than a single gene or other agent. Development of MS is likely to be influenced by the interactions of a number of genes, each of which (individually) has only a modest effect. Additional studies are needed to specifically pinpoint which genes are involved, determine their function, and learn how each gene's interactions with other genes and with the environment make an individual susceptible to MS.
Treatment
There is no known definitive cure for multiple sclerosis. However, several types of therapy have proven to be helpful. Different therapies are used for patients experiencing acute attacks, for patients who have the relapsing-remitting subtype, for patients who have the progressive subtypes, for patients without a diagnosis of MS who have a demyelinating event, and for managing the various consequences of MS attacks. Treatment is aimed at returning function after an attack, preventing new attacks, and preventing disability.
Currently only relapsing-remitting Multiple Sclerosis has FDA approved treatments. As of 2006 there are six Food and Drug Administration (FDA)-approved treatments for patients with relapsing-remitting MS. Three are interferons: Interferon beta-1a (Avonex and Rebif) or beta-1b (Betaseron [in Europe and Japan Betaferon]). The interferons are medications derived from human cytokines which help regulate the immune system. A fourth medication is glatiramer acetate (Copaxone), a mixture of polypeptides which may protect important myelin proteins by substituting itself as the target of immune system attack. The fifth medication, mitoxantrone is effective but is limited by cardiac toxicity. Finally, the sixth medication is Natalizumab (marketed as Tysabri).
Currently there are no approved treatments for the progressive varieties, though several medicaments are being studied and are described at Therapies for Multiple Sclerosis
Relapsing-remitting symptomatic attacks can be treated. Patients in the United States are typically given high doses of intravenous corticosteroids, such as methylprednisolone, to end the attack sooner and leave fewer lasting deficits.
Prognosis
The future course of the disease (or prognosis) for people with multiple sclerosis depends on the subtype of the disease, the individual's sex and race, their age, their initial symptoms, and the degree of disability they experience. The life expectancy of people with MS is now nearly the same as that of unaffected people. This is mainly due to improved methods of limiting disability, such as physical therapy and speech therapy, and more successful treatment of common complications of disability, such as pneumonia and urinary tract infections.
- Individuals with progressive subtypes of MS, particularly the primary progressive subtype, have a more rapid decline in function. In the primary progressive subtype, supportive equipment (such as a wheelchair or standing frame) is often needed after six to seven years. However, when the initial disease course is the relapsing-remitting subtype, the average time until such equipment is needed is twenty years. This means that many individuals with MS will never need a wheelchair.
- The earlier in life MS occurs, the slower disability progresses. Individuals who are older than fifty when diagnosed are more likely to experience a chronic progressive course, with more rapid progression of disability. Those diagnosed before age 35 have the best prognosis. Females generally have a better prognosis than males. Although black individuals tend to develop MS less frequently, they are often older at the time of onset and may have a worse prognosis.
- Initial MS symptoms of visual loss or sensory problems, such as numbness or tingling, are markers for a relatively good prognosis, whereas difficulty walking and weakness are markers for a relatively poor prognosis. Better outcomes are also associated with the presence of only a single symptom at onset, the rapid development of initial symptoms, and the rapid regression of initial symptoms.
- The degree of disability varies among individuals with MS. In general, one of three individuals will still be able to work after 15–20 years. Fifteen percent of people diagnosed with MS never have a second relapse, and these people have minimal or no disability after ten years. The degree of disability after five years correlates well with the degree of disability after fifteen years. This means that two-thirds of people with MS with low disability after five years will not get much worse during the next ten years. It should be noted that most of these outcomes were observed before the use of medications such as interferon, which can delay disease progression for several years.
Currently there are no clinically established laboratory investigations available that can predict prognosis or response to treatment. However, several promising approaches have been proposed. These include measurement of the two antibodies anti-myelin oligodendrocyte glycoprotein and anti-myelin basic protein, and measurement of TRAIL ( TNF-Related Apoptosis Inducing Ligand).
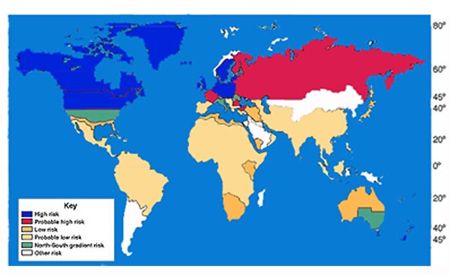
Epidemiology
In northern Europe, continental North America, and Australasia, about one of every 1000 citizens suffers from multiple sclerosis, whereas in the Arabian peninsula, Asia, and continental South America, the frequency is much lower. In sub-Saharan Africa, MS is extremely rare. With important exceptions, there is a north-to-south gradient in the northern hemisphere and a south-to-north gradient in the southern hemisphere, with MS being much less common in people living near the equator. Climate, diet, geomagnetism, toxins, sunlight exposure, genetic factors, and infectious diseases have all been discussed as possible reasons for these regional differences. Environmental factors during childhood may play an important role in the development of MS later in life. This idea is based on several studies of migrants showing that if migration occurs before the age of fifteen, the migrant acquires the new region's susceptibility to MS. If migration takes place after age fifteen, the migrant keeps the susceptibility of his home country. Additionally, smoking has been shown to be an independent risk factor for developing MS.
MS occurs mainly in Caucasians. It is twenty-fold lower in the Inuit people of Canada than in other Canadians living in the same region. It is also rare in the Native American tribes of North America, the Australian Aborigines and the Māori of New Zealand. These few examples point out that genetic background plays an important role in the development of MS.
As observed in many autoimmune disorders, MS is more common in females than males; the mean sex ratio is about two females for every male. In children (who rarely develop MS) the sex ratio may reach three females for each male. In people over age fifty, MS affects males and females equally. Onset of symptoms usually occurs between twenty to forty years of age, rarely before age fifteen or after age sixty.
As previously discussed, there is a genetic component to MS. On average one of every 25 siblings of individuals with MS will also develop MS. Almost half of the identical twins of MS-affected individuals will develop MS, but only one of twenty fraternal twins. If one parent is affected by MS, each child has a risk of only about one in forty of developing MS later in life.
History
A French neurologist named Jean-Martin Charcot (1825–93) was the first person to recognize multiple sclerosis as a distinct, separate disease in 1868. Summarizing previous reports and adding his own important clinical and pathological observations, Charcot called the disease sclerose en plaques. The three signs of MS now known as Charcot's triad are dysarthria (problems with speech), ataxia (problems with coordination), and tremor. Prior to Charcot, Robert Hooper (1773–1835), a British pathologist and practicing physician, Robert Carswell (1793–1857), a British professor of pathology, and Jean Cruveilhier (1791–1873), a French professor of pathologic anatomy, had described and illustrated many of the disease's clinical details.
There are several historical accounts of people who probably had MS. Saint Lidwina of Schiedam (1380–1433), a Dutch nun, may have been the first identifiable MS patient. From the age of sixteen until her death at age 53, she suffered intermittent pain, weakness of the legs, and vision loss—symptoms typical of MS. Augustus Frederick d'Este (1794–1848), an illegitimate grandson of King George III of Great Britain, almost certainly suffered from MS. D'Este left a detailed diary describing his 22 years living with the disease. His symptoms began at age 28 with a sudden transient visual loss after the funeral of a friend. During the course of his disease he developed weakness of the legs, clumsiness of the hands, numbness, dizziness, bladder disturbances, and erectile dysfunction. In 1844, he began to use a wheelchair. Despite his illness, he kept an optimistic view of life. Another early account of MS was kept by the British diarist W. N. P. Barbellion, who maintained a detailed log of his diagnosis and struggle with MS. His diary was published in 1919 as The Journal of a Disappointed Man.
Multiple sclerosis in film and television
The German propaganda film Ich klage an (1941) by Wolfgang Liebeneiner had the main character suffering from MS and wishing herself to be killed because she had become unable to do so by herself.
British cellist Jacqueline du Pré died of MS in 1987 after a long struggle with the disease, which robbed her of her capacity to perform as she progressively lost sensitivity in her fingers, muscle coordination, and her hearing. This decline was portrayed in the 1998 film, Hilary and Jackie. In "Duet For One," Julie Andrews plays a concert violinist who must sacrifice her career when she is diagnosed with MS.
In the American television series The West Wing, the fictional United States President, Josiah "Jed" Bartlet, has the relapsing-remitting subtype of MS. The storylines have educated many viewers about the nature of MS and have helped to dispel some of the misconceptions about the disease.
Another American TV series, Extreme Makeover: Home Edition, aired a two-part episode on February 12, 2006 that featured a new home for Carol Crawford-Smith of Blacksburg, Virginia, a former principal dancer with the Dance Theatre of Harlem who was diagnosed with MS in 2000. Ty Pennington and his team not only built her a new home, but also renovated her Blacksburg dance studio, "The Centre of Dance."