Vitamin D
2007 Schools Wikipedia Selection. Related subjects: Food and agriculture; General Chemistry
Vitamin D refers to a group of fat-soluble alcohols that contribute to the maintenance of normal levels of calcium and phosphorus in the blood. The two major forms of vitamin D are D2 (or ergocalciferol) and D3 or cholecalciferol. Vitamin D is required for the formation of strong bones and teeth. It is manufactured in the skin by the activation of a sterol (7-dehydrocholesterol) by ultraviolet radiation (sunlight). Vitamin D is classified as a vitamin because it is required for metabolism and deficiency can result in disease, including rickets and osteoporosis.
Overview
Vitamin D plays an important role in the maintenance of an intact and strong skeleton. The role traditionally attributed to the vitamin D system is to regulate the amount of calcium and phosphorus in the blood by ensuring correct intake from intestines and secretion. Vitamin D has also been implicated in a growing list of functions related to human biology.
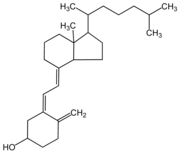
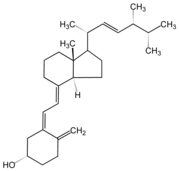
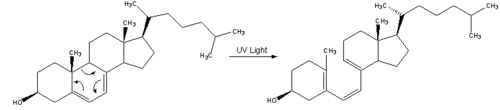
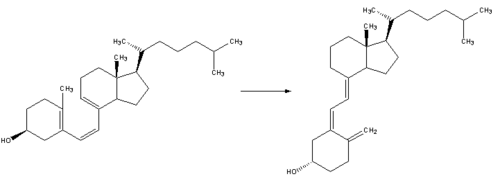
Vitamin D is produced in skin exposed to ultraviolet B radiation. The cholesterol precursor, 7-dehydrocholesterol, is unstable in UVB light, and the B-ring of the steroid structure breaks open to produce the seco-steroid, vitamin D3, more formally known as cholecalciferol. Diet is usually a minor secondary source of vitamin D, and even foods such as oily fish and eggs contain only very small amounts. It actualys plays the important role of acidic acid in the maintenance of preventing osteoperosis
Forms
- Vitamin D1: molecular compound of ergocalciferol with lumisterol, 1:1
- Vitamin D2: ergocalciferol or calciferol (made from ergosterol)
- Vitamin D3: cholecalciferol (made from 7-dehydrocholesterol). Cholecalciferol is the precursor of calcidiol, which in turn is the precursor of calcitriol
- Vitamin D4: 22,23-dihydroergocalciferol
- Vitamin D5: sitocalciferol (made from 7-dehydrositosterol)
Vitamin D2 is derived by irradiating fungi to produce ergocalciferol. Ergocalciferol does not naturally occur in the human body unless added by supplementation. In most mammals including humans, D3 is more effective than D2 at increasing 25-hydroxyvitamin D, the circulating reservoir of the vitamin D hormone. In the rat, D2 is more effective as a vitamin than D3, and in the squirrel monkey and the chick, D3 is more effective.
Vitamin D3, also known as cholecalciferol, is the form of vitamin D that is natural to all animal life, including human. It is made in the skin when 7-dehydrocholesterol reacts with UVB ultraviolet light with wavelengths 290 to 315 nm. This light is present in sunlight when the sun at sea level is more than 45 degrees above the horizon (when your shadow is no longer than you are tall, or when the UV index is more than 3). Typically, 10,000 IU (250 micrograms) can be made in the skin only after one minimal erythemal dose of exposure, or until the skin just begins to turn pink. An equilibrium is achieved in the skin when longer exposure to UVB simply degrades the product as fast as it is generated.
Biochemistry
Cholecalciferol is transported to the liver where it is hydroxylated to calcidiol or 25-hydroxy-vitamin D, the form of the vitamin that the body stores. A blood calcidiol level is the accepted way to determine vitamin D nutritional status. The optimal level of serum 25-hydroxyvitamin D remains a contentious point for debate among medical scientists. One recent consensus concludes that for optimal prevention of osteoporotic fracture the concentration should be higher than 30 ng/mL (US units), which is equal to 75 nmol/L (System International units).
The most active form of the vitamin is calcitriol (1,25 dihydroxy vitamin D3). This is both a potent hormone produced by the kidney and released into the circulation, and it is a paracrine/autocrine signalling molecule produced by many tissues for local regulation of cellular biology, but not released into the circulation. Calcitriol is synthesized from calcidiol in the kidneys to perform its endocrine function of maintaining the calcium economy. Calcitriol binds to a transcription factor which then regulates gene expression of transport proteins like TRPV6 and calbindin that are involved in calcium absorption in the intestine. The general result is the maintenance of calcium and phosphorus levels in the bone and blood with the assistance of parathyroid hormone and calcitonin.
Biochemically, the various forms of vitamin D, including calcidiol (25D) and calcitriol (1,25(OH)2D) are secosteroids; i.e. broken-open steroids. Secosteroids are very similar in structure to steroids except that two of the B-ring carbon atoms (C9 and 10) of the typical four steroid rings are not fused, whereas in steroids they are fused. Molecular modeling calculations suggest that at least in theory, vitamin D might have an affinity for several steroid receptors, including glucocorticoid and thyroid receptors.
Synthesis mechanism (form 3)
Nutrition
The U.S. Dietary Reference Intake (DRI) for an Adequate Intake (AI) for a 25-year old male for vitamin D is 5 micrograms/day (200 units/day). This rises to 15 micrograms/day (600 units/day) at age 70.
In food
At higher latitudes, total vitamin D input from sunlight is usually not sufficient, especially in the winter. To minimize risk of low serum 25-hydroxyvitamin D concentrations (the measure of vitamin D nutrition status), foods such as milk are often fortified with vitamin D2 or vitamin D3, typically giving 100 IU per glass. Fortified foods are the major dietary sources of vitamin D. Prior to the fortification of milk products with vitamin D in the 1930s, rickets, commonly caused by vitamin D deficiency, was a major public health problem. In the United States milk is fortified with 10 micrograms (400 IU) of vitamin D per quart, and rickets is now uncommon there.
One cup of vitamin D fortified milk supplies about one-fourth of the official estimated adequate intake of vitamin for adults older than age 50 years. Although milk is often fortified with vitamin D, dairy products made from milk (cheese, yogurt, ice cream, and so forth) are generally not. Only a few foods naturally contain significant amounts of vitamin D, including:
- Shiitake mushrooms, one of a few natural sources of vegan and kosher vitamin D (vitamin D2),
- Fish liver oils, such as cod liver oil, 1 Tbs. (15 mL), 1,360 IU (340% Daily value)
- Fatty fish, such as:
- Salmon, cooked, 3.5 oz, 360 IU (90% DV)
- Mackerel, cooked, 3.5 oz, 345 IU (90% DV)
- Sardines, canned in oil, drained, 1.75 oz, 250 IU (70% DV)
- Tuna, canned in oil, 3 oz, 200 IU (50% DV)
- Eel, cooked, 3.5 oz, 200 IU
- One whole egg, 20 IU (6% DV)
The U.S. Dietary Reference Intake Tolerable Upper Intake Level (UL) for a 25-year old male for vitamin D is 50 micrograms/day. This is equivalent to 2000 IU/day.
Diseases caused by deficiency
Vitamin D deficiency is known to cause several bone diseases including:
- Rickets: a childhood disease characterized by failure of growth and deformity of long bones.
- Osteoporosis: a condition characterized by fragile bones.
- Osteomalacia: a bone-thinning disorder in adults that is characterised by proximal muscle weakness and bone fragility. Osteomalacia can only occur in a mature skeleton.
The isolation of vitamin D and its functional role in rickets was determined by Edward Mellanby between 1918– 1920. The 1928 Nobel Prize was awarded to Adolf Windaus, who discovered the steroid, 7-dehydrocholesterol, the precursor of vitamin D.
Vitamin D malnutrition may be linked to chronic diseases such as cancer ( breast, ovarian, colon, prostate, lung and skin cancer), chronic pain, several autoimmune diseases, high blood pressure, depression, and seasonal affective disorder.
However, recent research indicates that in many chronic diseases where vitamin D levels (25 hydroxyvitamin D) appear to be low, vitamin D supplementation can actually cause long term harm. For example, supplementation with vitamin D is potentially hazardous for those with sarcoidosis and other diseases involving vitamin D hypersensitivity and dysregulation. There is increasing evidence for similar vitamin D hypersensitivity and dysregulation in a wide variety of autoimmune diseases, including rheumatoid arthritis and inflammatory bowel disease. Waterhouse et al reports vitamin D may appear to be low in these conditions, but only because it is being energetically converted to its active hormonal form (1,25 dihydroxyvitamin D) by disease processes.
Groups at greater risk
Older people (age 50 and over) have a higher risk of developing vitamin D deficiency. The ability of skin to convert 7-dehydrocholesterol to pre-vitamin D3 is decreased in older individuals. The kidneys, which help convert calcidiol to its active form, sometimes do not work as well when people age. Therefore, many older people may need vitamin D supplementation.
Newborn infants who are exclusively breastfed require vitamin D supplements. Breast milk does not contain significant levels of the vitamin, and although infants could receive this vitamin from sunlight, parents are usually advised to avoid exposing babies to open sunshine. The Canadian and American Pediatric Associations advise vitamin D supplementation from birth onwards, with 200 IU/day (5 mcg/d) in the south up to 800 IU/day in the north. Infant formula is generally fortified with vitamin D, so this requirement only applies to breastfed infants. Liquid "drops" of vitamin D for infants usually include vitamin A or other vitamins, and are available in pharmacies. These products are either detergent-solublized water based preparations (given at 0.5-1 mL/day) or oil-based preparations. Vitamin D as a single infant nutrient is also available in an oil that is given as one drop/day ("Baby Drops" in North America, or "Vigantol oil" in Europe).
Those who avoid or are not exposed to summer midday sunshine may also require vitamin D supplements. In particular, recent studies have shown Australians and New Zealanders are vitamin D deficient, particularly after the successful " Slip-Slop-Slap" health campaign encouraging Australians to cover up when exposed to sunlight to prevent skin cancer. Ironically, a vitamin D deficiency may also lead to skin cancer, although few minutes of exposure for light-skinned individuals may be all that is required; as the production of vitamin D is very rapid. However, the dermatology community contends that even a few minutes of unprotected ultraviolet exposure a day increases the risk of skin cancer and causes photoaging of the skin. Therefore, dermatologists are now recommending supplementation of vitamin D along with sunscreen use.
Dark-skinned individuals may require extra vitamin D because melanin acts like a sun-block, prolonging the time required to generate vitamin D. This does not pose a problem at latitudes below about 30 degrees, where the sunshine is so high in the sky all year that enough vitamin D is produced despite the dark skin colour. At higher latitudes, however, the decreased angle of the sun's rays, reduced daylight hours in winter, and protective clothing worn to guard against cold weather diminish absorption of sunlight and the production of vitamin D. Light-skinned people at higher latitudes also face these problems, but the lower amount of pigmentation in their skin allows more sunlight to be absorbed, thereby reducing the risk of vitamin D deficiency.
There is also evidence that obese people have lower levels of the circulating form of vitamin D, probably because it is deposited in body fat compartments and is less bioavailable, so obese people whose vitamin D production and intake is marginal or inadequate are at higher risk of deficiency. Patients with chronic liver disease or intestinal malabsorption may require larger doses of vitamin D (up to 40,000 IU or 1 mg (1000 micrograms) daily). To maintain blood levels of calcium, therapeutic vitamin D doses are sometimes administered (up to 100,000 IU or 2.5 mg daily) to patients who have had their parathyroid glands removed (most commonly renal dialysis patients who have had tertiary hyperparathyroidism, but also patients with primary hyperparathyroidism) or who suffer with hypoparathyroidism.
Overdose
Vitamin D in the human body has a large volume of distribution and a long half-life. In any case all common foods and correctly-formulated vitamin pills contain such small amounts of viatmin D that overdose could never occur under normal circumstances. Indeed, Stoss therapy involves taking a dose over a thousand times the daily RDA once every few months, and even then often fails to normalise vitamin D3 levels in the body. However, oral overdose has been recorded due to manufacturing and industrial accidents and leads to hypercalcaemia and atherosclerosis.
The exact long-term safe dose is not entirely known, but intakes of up to 2000 IU (10x the RDA) are believed to be safe, and some researchers believe that 10,000 IU does not lead to long term overdose. It seems that there are chemical processes that destroy excess vitamin D, even when taken orally, although these processes have not been identified (in experiments blood levels of vitamin D do not continue to increase over many months at these doses as presumably would be needed for toxicity to occur.) Although normal food and pill vitamin D concentration levels are too low to be toxic, because of the high vitamin A content in cod-liver oil (if taken in multiples of the normal dose) it is possible to reach poisonous levels .
Other research disputes the view that high vitamin D intake is benign. In one study, hypercalciuria and bone loss occurred at serum concentrations of 25D above approximately 50 ng/mL in patients supplementing with up to 3600 IU/day of D3. Another study showed elevated risk of ischaemic heart disease when 25D was above 89 ng/mL. In many chronic diseases, research indicates that vitamin D supplementation is inadvisable. There is increasing recognition that Th1 immune inflammation, occurring in rheumatic diseases can result in excessive numbers of activated macrophages converting 25-hydroxyvitamin D (25D) to its active 1,25 dihydroxyvitamin D (1,25D) hormonal form. This can lead to vitamin D dysregulation/hypersensitivity, which can lead to hypervitaminosis D, hypercalcemia and other symptoms. This is recognized as occurring in sarcoidosis and other diseases.
In cancer prevention and recovery
Research suggests that cancer patients who have their surgery or treatment in the summer — and therefore get more vitamin D — have a better chance of surviving than those who undergo treatment in the winter when they are exposed to less sunlight.
In 2005, U.S. scientists released a study, published in the American Journal of Public Health, which seems to demonstrate a beneficial correlation between vitamin D intake and prevention of cancer. Drawing from their meta-analysis of 63 published reports, the scientists claimed that an additional intake of 1,000 international units (IU) — or 25 micrograms — of the vitamin daily could lower an individual's cancer risk by 50% in colon cancer, and by 30% in breast and ovarian cancer. These are cross-sectional data, and thus the evidence is circumstantial. Longitudinal trials would be able to provide more conclusive proof of vitamin D's ability to prevent cancer.