Cholera
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
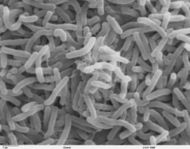
| Vibrio cholerae: The bacterium that causes cholera ( SEM image) | ||
| ICD- 10 | A 00. | |
| ICD- 9 | 001 | |
| DiseasesDB | 2546 | |
| MedlinePlus | 000303 | |
| eMedicine | med/351 ped/382 | |
| MeSH | C01.252.400.959.347 | |
Cholera is a water-borne disease caused by the bacterium Vibrio cholerae, which is typically ingested by drinking contaminated water, or by eating improperly cooked fish, especially shellfish. This phenomenon was first described in a scientific manner by the Portuguese physician Garcia de Orta in Colóquios dos Simples e Drogas da India ( 1563). Europe witnessed several epidemics in the 19th century, but the disease is since mostly seen in Third World countries, due to poor water infrastructure
Susceptibility
Recent epidemiologic research suggests that a person's susceptibility to cholera (and other diarrheas) is affected by their blood type. Those with type O blood are the most susceptible . Those with type AB are the most resistant, virtually immune. Between these two extremes are the A and B blood types, with type A being more resistant than type B .
About one million V. cholerae bacteria must be ingested to cause cholera in normally healthy adults, although increased susceptibility may be observed in those with a weakened immune system, individuals with decreased gastric acidity (as from the use of antacids), or those who are malnourished.
Transmission
V. cholerae occurs naturally in the plankton of fresh, brackish, and salt water, attached primarily to copepods in the zooplankton. Coastal cholera outbreaks typically follow zooplankton blooms. This makes cholera a zoonosis. Cholera is then transmitted through ingestion of feces contaminated with the bacterium. The contamination usually occurs when untreated sewage is released into waterways or into groundwater, affecting the water supply, any foods washed in the water, and shellfish living in the affected waterway — it is rarely spread directly from person to person.
The resulting diarrhea allows bacteria to spread to other people under unsanitary conditions.
Symptoms
Symptoms include those of general GI tract upset, including profuse diarrhea. Symptoms are caused by the enterotoxins that V. cholerae produces. The main enterotoxin, known as cholera toxin, interacts with G proteins and cyclic AMP in the intestinal lining to open ion channels. As ions flow into the intestinal lumen, water follows due to osmosis.
Famous cholera victims
The crying and pathos in the last movement of Tchaikovsky's last symphony made people think that Tchaikovsky had a premonition of death. "A week after the premiere of his Sixth Symphony, Tchaikovsky was dead.... The cause of this indisposition and stomach ache was suspected to be his infecting himself with cholera by drinking contaminated water. The day before while having lunch with Modest (his brother and biographer), he is said to have poured faucet water from a pitcher into his glass and drunk a few swallows. Since the water was not boiled and cholera was once again rampaging St. Petersburg, such a connection was quite plausible ...."
Other famous people who succumbed to the disease include:
- James K. Polk
- Nicolas Léonard Sadi Carnot
- Georg Wilhelm Friedrich Hegel
- Samuel Charles Stowe, son of Harriet Beecher Stowe
- Carl von Clausewitz
- George Bradshaw
- Adam Mickiewicz
- August von Gneisenau
- William Jenkins Worth
- John Blake Dillon
- Daniel Morgan Boone, founder of Kansas City, Missouri, son of Daniel Boone
- James Clarence Mangan
- Juan de Veramendi, Mexican Governor of Texas, father-in-law of Jim Bowie
- Grand Duke Constantine Pavlovich of Russia
- William Shelley, son of Mary Shelley
- William Godwin, brother of Mary Shelley
- Judge Daniel Stanton Bacon, father-in-law of George Armstrong Custer
- Inessa Armand, mistress of Lenin and the mother of Andre, his son.
Alexandre Dumas, French author of The Three Musketeers and The Count of Monte Cristo, also contracted cholera in the 1832 Paris epidemic and almost died, before he wrote these two novels.
Biochemistry of the V. cholerae bacterium
Most of the Vibrio cholerae bacteria in the water that a potential host drinks do not survive the very acidic conditions of the human stomach But the few bacteria that manage to survive the stomach's acidity conserve their energy and stored nutrients during the perilous passage through the stomach by shutting down much protein production. When the surviving bacteria manage to exit the stomach and reach the favorable conditions of the small intestine, they need to propel themselves through the thick mucus that lines the small intestine to get to the intestinal wall where they can thrive. So they start up production of the hollow cylindrical protein flagellin to make flagella, the curly whip-like tails that they rotate to propel themselves through the pasty mucus that lines the small intestine.
But when the cholera bacteria reach the intestinal wall, they do not need the flagella propellers to move themselves any more, so they stop producing the protein flagellin, thus again conserving energy and nutrients by changing the mix of proteins that they manufacture, responding to the changed chemical surroundings. And on reaching the intestinal wall, they start producing the toxic proteins that give the infected person a watery diarrhea which carries the multiplying and thriving new generations of V. cholerae bacteria out into the drinking water of the next host—if proper sanitation measures are not in place.
Microbiologists have studied the genetic mechanisms by which the V. cholerae bacteria turn off the production of some proteins and turn on the production of other proteins as they respond to the series of chemical environments they encounter, passing through the stomach, through the mucous layer of the small intestine, and on to the intestinal wall. Of particular interest have been the genetic mechanisms by which cholera bacteria turn on the protein production of the toxins that pull chloride ions and accompanying water from the host's blood supply into the small intestine to create the sickening diarrhea. The host can become rapidly dehydrated if an appropriate mixture of dilute salt water and sugar is not taken to replace the blood's water and salts lost in the diarrhea.
By inserting separately successive sections of V. cholerae DNA into the DNA of other bacteria such as E. Coli that would not naturally produce the protein toxins, researchers could find out the separate pieces of the mechanisms by which V. cholerae respond to the changing chemical environments of the stomach, mucous layers, and intestinal wall. Researchers discovered that there is a complex cascade of regulatory proteins that control expression of V. cholerae virulence determinants. In responding to the chemical environment at the intestinal wall, the V. cholerae bacteria produce the TcpP/TcpH proteins which, together with the ToxR/ToxS proteins, activate the expression of the ToxT regulatory protein. ToxT then directly activates expression of virulence genes that produce the toxins that cause diarrhea in the infected person and that permit the bacteria to colonize the intestine. Current research aims at discovering "the signal that makes the cholera bacteria stop swimming and start to colonize (that is, adhere to the cells of) the small intestine."
History
Origin and Spread
Cholera was originally endemic to the Indian subcontinent, with the Ganges River likely serving as a contamination reservoir. It spread by trade routes (land and sea) to Russia, then to Western Europe, and from Europe to North America. It is now no longer considered an issue in Europe and North America, due to filtering and chlorination of the water supply.
- 1816-1826 - First pandemic: Previously restricted, the pandemic began in Bengal, then spread across India by 1820. It extended as far as China and the Caspian Sea before receding.
- 1829-1851 - Second pandemic reached Europe, London and Paris in 1832. In London, it claimed 6536 victims; in Paris, 20,000 succumbed (out of a population of 650,000) with 100,000 victims in all of France . It reached Russia ( Cholera Riots), Quebec, Ontario and New York in the same year and the Pacific coast of North America by 1834.
- 1849 - Second outbreak in Paris. In London, it was the worst outbreak in the city's history, claiming 14,137 lives. An outbreak in North America took the life of former U.S. President James K. Polk
- 1852-1860 - Third pandemic mainly affected Russia, with over a million deaths. In 1853-4, London's epidemic claimed 10,738 lives.
- 1854 - Outbreak of cholera in Chicago took the lives of 5 1/2 per cent of the population
- 1863-1875 - Fourth pandemic spread mostly in Europe and Africa.
- 1866 - Outbreak in North America. In London, a localised epidemic in the East claimed 5,596 lives.
- 1899-1923 - Sixth pandemic had little effect in Europe because of advances in public health, but Russia was badly affected again.
- 1961-1970s - Seventh pandemic began in Indonesia, called El Tor after the strain, and reached Bangladesh in 1963, India in 1964, and the USSR in 1966. From North Africa it spread into Italy by 1973. In the late 1970s there were small outbreaks in Japan and in the South Pacific. There were also many reports of a cholera outbreak near Baku in 1972, but information of this was suppressed in the USSR.
- January 1991 to September 1994 - Outbreak in South America, apparently initiated by discharged ballast water. Beginning in Peru there were 1.04 million identified cases and almost 10,000 deaths. The causative agent was a non-O1, nonagglutinable vibrio (NAG) named O139 Bengal. It was first identified in Tamilnadu, India and for a while displaced El Tor in southern Asia before decreasing in prevalence from 1995 to around 10% of all cases. It is considered to be an intermediate between El Tor and the classic strain and occurs in a new serogroup. There is evidence as to the emergence of wide-spectrum resistance to drugs such as trimethoprim, sulfamethoxazole and streptomycin.
Research
The scientists with major contributions to fighting cholera were John Snow, who found the link between cholera and drinking water in 1854, and Robert Koch, who identified V. cholerae as the bacillus causing the disease. The bacterium was originally isolated thirty years earlier by Italian anatomist Filippo Pacini, but his results were not widely known around the world. However John Snow and Robert Koch didn't know of Pacini's previous success and so were widely credited for the breakthrough.
Cholera has been a laboratory for the study of evolution of virulence. The province of Bengal in British India was partitioned into West Bengal (a state in India) and the nation of Bangladesh in 1947. Prior to partition, both regions had Cholera pathogens with similar characteristics. After 1947, India made more progress on public health than Bangladesh. As a consequence, the strains of the pathogen which succeeded in India had a greater incentive in the longevity of the host, and are less virulent than the strains prevailing in Bangladesh, which uninhibitedly draw upon resources of the host thus rapidly killing him.
Other historical information
In the past, people travelling in ships would hang a yellow flag if one or more of the crew members suffered from cholera. Boats with a yellow flag hung would not be allowed to disembark at any harbour. (See Love in the Time of Cholera)
Treatment
Treatment typically consists of aggressive rehydration and replacement of electrolytes, since the death rate is generally high due to the serious dehydration caused by the illness.
Tetracycline antibiotics may have a role in reducing the duration and severity of cholera, although drug-resistance is occurring, and their effects on overall mortality is questioned. Other antibiotics that have been used include ciprofloxacin and azithromycin.
Prevention
Although cholera can be life-threatening, it is easily prevented. In the United States and Western Europe, because of advanced water and sanitation systems, cholera is not a major threat. The last major outbreak of cholera in the United States was in 1911. However, everyone, especially travellers, should be aware of how the disease is transmitted and what can be done to prevent it.
Simple sanitation is usually sufficient to stop an epidemic. There are several points along the transmission path at which the spread may be halted:
- Sickbed: Proper disposal and treatment of waste produced by cholera victims.
- Sewage: Treatment of general sewage before it enters the waterways.
- Sources: Warnings about cholera contamination posted around contaminated water sources.
- Sterilization: Boiling, filtering, and chlorination of water before use.
Filtration and boiling is by far the most effective means of halting transmission. Cloth filters, though very basic, have greatly reduced the occurrence of cholera when used in poor villages in Bangladesh that rely on untreated surface water.
In general, education and sanitation are the limiting factors in prevention of cholera epidemics.
Trivia
- A persistent but false urban legend states that 90,000 people died in Chicago of cholera and typhoid fever in 1885. This story has no factual basis.