Blood type
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
A total of 29 human blood group systems are recognized by the International Society of Blood Transfusion (ISBT). The most important of these are the ABO blood group system and the Rhesus blood group system.
Each blood group is represented by a substance on the surface of red blood cells (RBCs). These substances are important because they contain specific sequences of amino acid and carbohydrate which are antigenic. As well as being on the surface of RBCs, some of these antigens are also present on the cells of other tissues. A complete blood type describes the set of 29 substances on the surface of RBCs, and an individual's blood type is one of the many possible combinations of blood group antigens; usually only the ABO blood group system and the presence or absence of the Rhesus D antigen (also known as the Rhesus factor) are determined and used to describe the blood type. Over 600 different blood group antigens have been found, many of these being very rare. If an individual is exposed to a blood group antigen that is not recognised as self, the individual can become sensitized to that antigen; the immune system makes specific antibodies which binds specifically to a particular blood group antigen and an immunological memory against that particular antigen is formed. These antibodies can bind to antigens on the surface of transfused red blood cells (or other tissue cells) often leading to destruction of the cells by recruitment of other components of the immune system. Knowledge of an individual's blood type is important to identify appropriate blood for transfusion or tissue for organ transplantation.
Several different RBC surface antigens stemming from one allele (or very closely linked genes) are collectively labeled as a blood group system (or blood group). The two most important blood group systems were discovered during early experiments with blood transfusion, the ABO group in 1901 and the Rhesus group in 1937. These two blood groups are reflected in the common nomenclature A positive, O negative, etc. with letters referring to the ABO group and positive/negative to the presence/absence of the RhD antigen of the Rhesus group. Development of the Coombs test in 1945 and the advent of transfusion medicine led to discovery of more blood groups. The Coombs test is used routinely in the screening of blood for blood group antibodies in the preparation of blood for transfusion.
Blood types are inherited and represent contributions from both parents. Some blood types are rare, and are primarily found in certain ethnic groups. Some blood types are associated with inheritance of other diseases, for example the Kell antigen is associated with McLeod syndrome. Certain blood types may affect susceptibility to infections, an example being the resistance to specific malaria species seen in individuals lacking the Duffy antigen. Very rarely, a person's blood type changes through addition or suppression of an antigen in infection or malignancy. Transfusion reactions can occur if a person is transfused with blood of a different blood type. Mismatches involving minor antigens or weak antibodies may lead to minor problems; however, more serious incompatibilities can lead to a more vigorous immune response with massive RBC destruction, low blood pressure, and even death.
Often, pregnant women carry a fetus with a different blood type to their own, and sometimes the mother forms antibodies against the red blood cells of the fetus, which causes hemolysis of fetal RBCs and leads to low fetal blood counts, a condition known as hemolytic disease of the newborn.
Introduction
ABO and Rhesus: the two main blood group systems
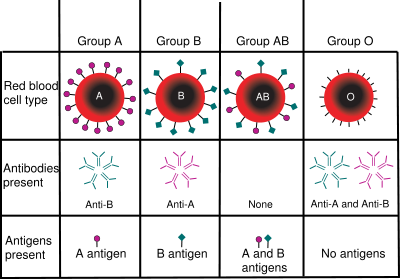
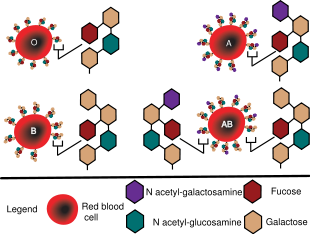
The ABO system is the most important blood group system in human blood transfusion. The associated anti-A antibodies and anti-B antibodies are usually IgM antibodies. ABO IgM antibodies are produced in the first years of life by sensitization to environmental substances such as food, bacteria and viruses. The "O" in ABO is often replaced by 0 (zero/null) in other languages.
The Rhesus system is the second most important blood group system in human blood transfusion. The most important Rhesus antigen is the RhD antigen because it is the most immunogenic of the five main rhesus antigens; however, anti-RhD antibodies are not usually produced by sensitization against environmental substances. It is common for RhD negative individuals not to have any anti-RhD IgG or IgM antibodies; nevertheless, RhD negative individuals can produce IgG antibodies when they are transfused with RhD positive RBCs.
The agglutination of IgM is stronger due to the relatively large size of the IgM antibody, but the nature of the bodily reaction as a result of agglutination with IgG can be more dramatic
Table of ABO and Rh distribution by nation
| Population | O+ | A+ | B+ | AB+ | O− | A− | B− | AB− |
|---|---|---|---|---|---|---|---|---|
| Australia | 40% | 31% | 8% | 2% | 9% | 7% | 2% | 1% |
| Canada | 39.0% | 36.0% | 7.6% | 2.5% | 7.0% | 6.0% | 1.4% | 0.5% |
| Denmark | 35% | 37% | 8% | 4% | 6% | 7% | 2% | 1% |
| Finland | 27% | 38% | 15% | 7% | 4% | 6% | 2% | 1% |
| France | 36% | 37% | 9% | 3% | 6% | 7% | 1% | 1% |
| Korea, South | 27.4% | 34.4% | 26.8% | 11.2% | 0.1% | 0.1% | 0.1% | 0.05% |
| Sweden | 32% | 37% | 10% | 5% | 6% | 7% | 2% | 1% |
| UK | 37% | 35% | 8% | 3% | 7% | 7% | 2% | 1% |
| USA | 38% | 34% | 9% | 3% | 7% | 6% | 2% | 1% |
Other human blood group systems
The International Society of Blood Transfusion currently recognizes 29 blood group systems (including the ABO and Rh systems). Thus, in addition to the ABO antigens and Rhesus antigens, many other antigens are expressed on the RBC surface membrane. For example, an individual can be AB RhD positive, and at the same time M and N positive (MNS system), K positive (Kell system), Lea or Leb positive (Lewis system), and so on for each blood group system. Many of the blood group systems were named after the patients in whom the corresponding antibodies were initially encountered.
Importance for transfusions
Transfusion medicine is a specialized branch of hematology that is concerned with the study of blood group antigens and blood group antibodies, along with the work of a blood bank to provide a transfusion service for blood and other blood products. Across the world blood products must be prescribed by a medical doctor (licensed physician or surgeon) in a similar way to medicines. In the USA blood products are tightly regulated by the Food and Drug Administration.
Blood transfusions between donor and recipient of incompatible blood types can cause severe acute immunological reactions, hemolysis (RBC destruction), renal failure, shock, and sometimes death. Antibodies can be highly active and can attack RBCs and bind components of the complement system to cause massive hemolysis of the transfused blood.
Hemolytic disease of the newborn
An antenatal woman can make IgG blood group antibodies if her fetus has a blood group antigen that she does not. This can happen if some of the fetus' blood cells pass into the mother's blood circulation (e.g. a small fetomaternal hemorrhage at the time of child birth) or sometimes after a therapeutic blood transfusion. This can lead to Rh disease or another forms of hemolytic disease of the newborn (HDN) in her current baby or in subsequent pregnancies. Some blood groups can cause severe HDN, some can only cause mild HDN and others are not known to cause HDN.
Compatibility
Blood products
In order to provide maximum benefit from each blood donation and to extend shelf-life, blood banks fractionate whole blood into several products. The most common of these products are packed RBCs, plasma, platelets, cryoprecipitate, and fresh frozen plasma (FFP). FFP is quick-frozen to retain labile clotting factors V and VIII and usually administered to patients who have a potentially fatal clotting problem caused by a condition such as advanced liver disease, overdose of anticoagulant, or disseminated intravascular coagulation (DIC).
Clotting factors synthesized by modern recombinant methods are now in routine clinical use for hemophilia, as the risks of infection transmission that occur with pooled blood products are avoided.
Cross matching blood
Patients should ideally receive their own blood or type-specific blood products to minimize the chance of a transfusion reaction. If time allows, the risk will further be reduced by cross-matching blood, in addition to blood typing both recipient and donor. Cross-matching involves mixing a sample of the recipient's blood with a sample of the donor's blood and checking to see if the mixture agglutinates, or forms clumps. Blood bank technicians usually check for agglutination with a microscope, and if it occurs, that particular donor's blood cannot be transfused to that particular recipient. Blood transfusion is a potentially risky medical procedure and it is vital that all blood specimens are correctly identified, so in cross-matching labeling is standardized using a barcode system known as ISBT 128.
RBC compatibility
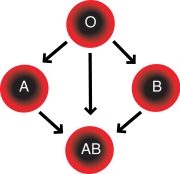
- Blood group AB individuals have both A and B antigens on the surface of their RBCs, and their blood serum does not contain any antibodies against either A or B antigen. Therefore, an individual with type AB blood can receive blood from any group (with AB being preferable), but can only donate blood to another group AB individual.
- Blood group A individuals have the A antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the B antigen. Therefore, a group A individual can only receive blood from individuals of groups A or O (with A being preferable), and can donate blood to individuals of groups A or AB.
- Blood group B individuals have the B antigen on their surface of their RBCs, and blood serum containing IgM antibodies against the A antigen. Therefore, a group B individual can only receive blood from individuals of groups B or O (with B being preferable), and can donate blood to individuals of groups B or AB.
- Blood group O (or blood group zero in some countries) individuals do not have either A or B antigens on the surface of their RBCs, but their blood serum contains IgM antibodies against both A and B antigens. Therefore, a group O individual can only receive blood from a group O individual, but they can donate blood to individuals of any ABO blood group (ie A, B, O or AB). O- is therefore used when an emergency transfusion is necessary and there has not been enough time to verify the patient's blood type.
| Recipient blood type | Donor must be | |||||||
|---|---|---|---|---|---|---|---|---|
| AB+ | Any blood type | |||||||
| AB- | O- | A- | B- | AB- | ||||
| A+ | O- | O+ | A- | A+ | ||||
| A- | O- | A- | ||||||
| B+ | O- | O+ | B- | B+ | ||||
| B- | O- | B- | ||||||
| O+ | O- | O+ | ||||||
| O- | O- | |||||||
An RhD negative patient (who has not been sensitized to RhD positive RBCs and who does not have any anti-D antibodies) can receive RhD positive blood cells, but there is a high probability that this would sensitize the patient to the RhD antigen, and a female patient would risk HDN. Therefore RhD positive blood is never given to RhD negative women of childbearing age, and is only given to other RhD negative patients in extreme circumstances, such as a major bleed when RhD negative red cells are running short. If a RhD negative patient has developed anti-D antibodies, a second exposure to RhD positive blood would lead to a potentially dangerous transfusion reaction. Occasionally, for transfusion of males or women above child-bearing age, RhD positive blood is given to a RhD negative individual (who do not have atypical red cell antibodies) when it is necessary to conserve RhD negative blood stocks in the blood bank for use in people where sensitisation to RhD antigens could cause serious problems. The converse is not true: RhD positive patients do not react to RhD negative blood.
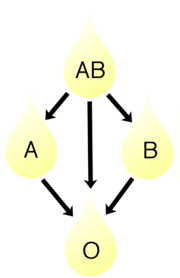
Plasma compatibility
Donor-recipient compatibility for blood plasma is the reverse from that of RBCs. Plasma extracted from type AB blood can be transfused to individuals of any blood group, but type O plasma can only be used by type O recipients.
Rhesus D antibodies are not usually naturally occurring, so generally both RhD negative and RhD positive blood do not contain anti-RhD antibodies. RhD negative or RhD positive donor blood plasma can therefore generally be transfused into both RhD negative and RhD positive recipients. Consequently RhD positive or RhD negative is irrelevant in the table below. If anti-RhD antibodies have developed in a donor these would be detected by antibody screening in the blood bank. Donor blood containing anti-RhD antibodies would not be suitable for transfusion into a RhD positive patient, but anyone with any strong atypical blood group antibodies would not be accepted as a blood donor.
| Recipient blood type | Donor must be | |||
|---|---|---|---|---|
| AB | AB | |||
| A | A or AB | |||
| B | B or AB | |||
| O | Any blood type | |||
Universal donors and universal recipients
Individuals with blood type O negative are often called universal donors and individuals with type AB positive blood are called universal recipients, but the terms universal donor and universal recipient are not very useful, because they only consider the reaction of the patient's antibodies to received red blood cells, and not the antibodies present in the transfused blood. These terms may be generally true for transfusions of packed red cells, where as much of the plasma as possible has been removed. Thus, although a transfusion of O negative blood to a patient of blood group A or B is unlikely to produce an immune reaction due to the recipient's antibodies, the transfused blood may itself contain antibodies to the patient's A and B antigens; this can cause an adverse reaction, although the risk is far less than that of an O negative patient receiving types A or B. For this reason an exact ABO-type match is preferable where circumstances allow. Additionally, the other red blood cell surface antigens that belong to blood groups other than the ABO blood group system might cause an adverse reaction if they can bind the corresponding antibodies.
With respect to transfusions of plasma this situation is reversed. Type O plasma can only be given to O recipients, while AB plasma (which does not contain anti-A or anti-B antibodies) can be given to patients of any ABO blood group.
Transfusions are further complicated because platelets and white blood cells (WBCs) have their own systems of surface antigens. Sensitization to platelet or WBC antigens can occur as a result of transfusion.