Sickle-cell disease
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
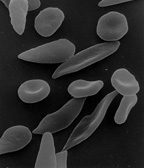
| Sickle-shaped red blood cells | ||
| ICD- 10 | D 57. | |
| ICD- 9 | 282.6 | |
| OMIM | 603903 | |
| DiseasesDB | 1206 | |
| MedlinePlus | 000527 | |
| eMedicine | emerg/26 | |
| MeSH | C15.378.071.141.150.150 | |
Sickle-cell disease is a general term for a group of genetic disorders caused by sickle hemoglobin (Hgb S or Hb S). In many forms of the disease, the red blood cells change shape, usually looking much like that of a banana, upon deoxygenation because of polymerization of the abnormal sickle hemoglobin. This process damages the red blood cell membrane, and can cause the cells to become stuck in blood vessels. This deprives the downstream tissues of oxygen and causes ischemia and infarction. The disease is chronic and lifelong. Individuals are most often well, but their lives are punctuated by periodic painful attacks. In addition to periodic pain, there may be damage of internal organs, such as stroke. Lifespan is often shortened with sufferers living to an average of 40 years. Sickle-cell disease occurs more commonly in people (or their descendants) from parts of the world, such as sub-Saharan Africa, where malaria is or was common. Sickle-cell disease can occur in any individual of any colour or ethnicity, however.
Types and terminology
"Sickle-cell anaemia" is the name of a specific form of sickle-cell disease in which there is homozygosity for the mutation that causes Hgb S. Other forms of sickle-cell disease include:
- sickle-haemoglobin C disease
- sickle beta-plus-thalassemia
- sickle beta-zero-thalassemia
- hemoglobin ss
Unlike sickle-cell anaemia, these other forms of sickle-cell disease are compound heterozygous states in which the person has only one copy of the mutation that causes Hgb S and one copy of another abnormal haemoglobin gene. It is important to know that "sickle-cell anaemia" is the proper name of a specific type of "sickle-cell disease", and that "sickle-cell disease" is a non-specific term. Because the different forms of sickle-cell disease are quite different, one must be sure to specify the exact form of the disease in question.
Signs and symptoms
Patients with sickle cell anaemia have an anaemia that varies in severity, with typical hemoglobin levels of 6-9 g/dl. Reticulocyte counts are elevated, reflecting new red blood cells replacing the rapidly destroyed older cells - red blood cell life span is markedly reduced in this disease. Often, the white blood cell and platelet counts are elevated, and these cells may contribute to vaso- occlusion.
Vaso-occlusive crises
A vaso-occlusive crisis is caused by sickle-shaped red blood cells that obstruct capillaries and restrict bloodflow to an organ, resulting in ischemia, pain, and organ damage.
Because of its narrow vessels and function in clearing defective red blood cells, the spleen is frequently affected. It is usually infarcted before the end of childhood in individuals suffering from sickle-cell anaemia. This autosplenectomy increases the risk of infection from encapsulated organisms; preventive antibiotics and vaccinations are recommended for those with such asplenia. Liver failure may also occur with time.
Bones, especially weight-bearing bones, are also a common target of vasoocclusive damage. Such damage may result -cell patients is also due to the bone ischemia.
A recognized type of sickle crisis is the acute chest crisis, a condition characterized by fever, chest pain, hard breathing, and pulmonary infiltrate on chest X-ray. Given that pneumonia and intra-pulmonary sickling can both produce these symptoms, the patient is treated for both conditions. Treatment consists of admission, oxygen, close monitoring, and intravenous antibiotics.
Other sickle-cell crises
- Aplastic crisis. An acute worsening of the patient's baseline anaemia producing pallor, tachycardia, and fatigue. This crisis is triggered by parvovirus B19, which directly affects erythropoiesis (production of red blood cells). Reticulocyte counts drop dramatically during the illness and the rapid turnover of red cells leads to the drop in hemoglobin. Most patients can be managed supportively; some need blood transfusion.
- Splenic sequestration crisis. An acute, painful enlargement of the spleen. The abdomen becomes bloated and very hard. Management is supportive, sometimes with blood transfusion.
Complications
Sickle-cell anaemia can lead to various complications, including:
- Vaso-occlusive crisis (otherwise known as pain crisis): Most patients with sickle cell disease have periodic intensely painful episodes called vaso-occlusive crises. The frequency, severity, and duration of these crises vary tremendously. Painful crises are treated with hydration and analgesics; pain management requires opioid administration at regular intervals until the crisis has settled. For milder crises a subgroup of patients manage on NSAIDs (such as diclofenac or naproxen). For more severe crises most patients require inpatient management for intravenous opioids; patient-controlled analgesia (PCA) devices are commonly used in this setting. Diphenhydramine is effective for the itching associated with the opioid use. Incentive spirometry, a technique to encourage deep breathing to minimize the development of atelectasis, is recommended.
- Acute chest syndrome: Acute chest syndrome is a life-threatening condition characterized by chest pain, shortness of breath, fever, hypoxemia, and pulmonary infiltrates on chest X-ray. It can be triggered by pain crisis, respiratory infection, bone-marrow embolization, or possibly by atelectasis, such as can be caused by opiate administration, or surgery.
- Overwhelming post-(auto)splenectomy infection - due to functional asplenia, caused by encapsulated organisms such as Streptococcus pneumoniae and Haemophilus influenzae. Daily penicillin prophylaxis is the most commonly used treatment during childhood with some hematologists continuing treatment indefinitely. Patients benefit today from routine vaccination for Haemophilus influenzae, Pneumococcus and Meningococcus.
- Stroke - progressive vascular narrowing (occlusion) can prevent oxygen from reaching the brain, leading to stroke; cerebral infarction occurs in children, and cerebral hemorrhage in adults.
- Cholelithiasis and cholecystitis (gallstones) - prolonged hemolysis may lead to excessive bilirubin production and precipitation, leading to gallstones
- Avascular necrosis ( aseptic bone necrosis) of the hip
- Decreased immune reactions due to hyposplenism (malfunctioning of the spleen)
- Priapism and infarction of the penis (in men)
- Osteomyelitis (bacterial bone infection) - salmonella is noted much more commonly than in the general population, but staphylococcus is still the most common pathogen.
- Opioid addiction (see below)
Diagnosis
Attacks are diagnosed clinically, i.e. there is no gold standard diagnostic test. Hemolysis (anaemia and jaundice) is often present, although for painful crises the diagnosis depends essentially on how the patient describes the pain.
Abnormal hemoglobin forms are detected on hemoglobin electrophoresis, a form of gel electrophoresis on which the various types of hemoglobin move at varying speed. Sickle cell hemoglobin (HbSS) and Hemoglobin C with sickling (HbSC)—the two most common forms—can be identified from there. Genetic testing is rarely performed.
Pathophysiology
Sickle-cell anaemia is caused by a missense mutation in the β-globin chain of hemoglobin, replacing the amino acid glutamic acid with the less polar amino acid valine at the sixth position of the β chain . The association of two wild type α-globin subunits with two mutant β-globin subunits forms hemoglobin S, which polymerises under low oxygen conditions causing distortion of red blood cells and a tendency for them to lose their elasticity.
New erythrocytes are quite elastic, which allows the cells to deform to pass through capillaries. Often a cycle occurs because as the cells sickle, they cause a region of low oxygen concentration which causes more red blood cells to sickle. Repeated episodes of sickling causes loss of this elasticity and the cells fail to return to normal shape when oxygen concentration increases. These rigid red blood cells are unable to flow through narrow capillaries, causing vessel occlusion and ischemia.
Genetics
The allele responsible for sickle cell anaemia is autosomal recessive. A person who receives the defective gene from both father and mother develops the disease; a person who receives one defective and one healthy allele remains healthy, but can pass on the disease and is known as a carrier. If two parents who are carriers have a child, there is a 1-in-4 chance of their child developing the illness and a 1-in-2 chance of their child just being a carrier.
The gene defect is a known mutation of a single nucleotide (A to T) of the β-globin gene, which results in glutamic acid to be substituted by valine at position 6. Hemoglobin S with this mutation are referred to as HbS, as opposed to the normal adult HbA. The genetic disorder is due to the mutation of a single nucleotide, from a GAG to GTG codon mutation. This is normally a benign mutation, causing no apparent effects on the secondary, tertiary, or quaternary structure of hemoglobin. What it does allow for, under conditions of low oxygen concentration, is the polymerization of the HbS itself. The deoxy form of hemoglobin exposes a hydrophobic patch on the protein between the E and F helices. The hydrophobic residues of the valine at position 6 of the beta chain in hemoglobin are able to bind to the hydrophobic patch, causing hemoglobin S molecules to aggregate and form fibrous precipitates. In people heterozygous for HbS (carriers of sickling hemoglobin), the polymerization problems are minor. In people homozygous for HbS, the presence of long chain polymers of HbS distort the shape of the red blood cell, from a smooth donut-like shape to ragged and full of spikes, making it fragile and susceptible to breaking within capillaries. Carriers only have symptoms if they are deprived of oxygen (for example, while climbing a mountain) or while severely dehydrated. For those afflicted with the disease, however, vasocclusive events can be a painful part of life (normally they occur 0.8 times per year per patient). This occurs when HbS becomes deoxygenated it undergoes an abnormal change in shape and consistency which can lead to a change in the shape and plasticity in the cell wall of the RBC, an occurrence called sickling.
The sufferers of the illness have a reduced life span. It is believed that carriers ( sickle cell trait) are relatively resistant to malaria. Since the gene is incompletely recessive, carriers have a few sickle red blood cells at all times, not enough to cause symptoms, but enough to give resistance to malaria. Because of this, heterozygotes have a higher fitness than either of the homozygotes. This is known as heterozygote advantage.
The malaria parasite has a complex life cycle and spends part of it in red blood cells. In a carrier, the presence of the malaria parasite causes the red blood cell to rupture, making the plasmodium unable to reproduce. Further, the polymerization of Hb affects the ability of the parasite to digest Hb in the first place. Therefore, in areas where malaria is a problem, people's chances of survival actually increase if they carry sickle cell trait (selection for the heterozygote).
Due to the above phenomenon, the illness is still prevalent, especially among people with recent ancestry in malaria-stricken areas, such as Africa, the Mediterranean, India and the Middle East. In fact, sickle-cell anaemia is the most common genetic disorder among African Americans; about 1 in every 12 is a carrier.
The evolution of sickle-cell anaemia is probably an example of Baldwinian evolution, whereby humans modify their environment and thus change the selective pressures. As humans in tropical areas in Africa and elsewhere developed agriculture and animal husbandry, they expanded the niche for Anopheles mosquitoes that could transmit the malaria parasite.
In the USA, where there is no endemic malaria, the incidence of sickle cell anaemia amongst African Americans is much lower than in West Africa and falling. Without endemic malaria from Africa, the condition is purely disadvantageous, and will tend to be bred out of the affected population. See the Price equation article for a simplified mathematical model of the genetic evolution of sickle cell anaemia.
Inheritance
Sickle cell conditions are inherited from parents in much the same way as blood type, hair color and texture, eye colour and other physical traits. The types of hemoglobin a person makes in the red blood cells depend upon what hemoglobin genes the person inherits from his or her parents. Like most genes, hemoglobin genes are inherited in two sets, one from each parent.
Examples
- If one parent has Sickle Cell Anaemia ("rr" in the diagram above) and the other is Normal (RR), all of their children will have sickle cell trait (Rr).
- If one parent has Sickle Cell Anaemia (rr) and the other has Sickle Cell Trait (Rr), there is a 50% chance (or 1 out of 2) of a child having sickle cell disease (rr) and a 50% chance of a child having sickle cell trait (Rr).
- When both parents have Sickle Cell Trait (Rr), they have a 25% chance (1 of 4) of a child having sickle cell disease (rr), as shown in the diagram above.
Treatment
Febrile illness
Children with fever are screened for bacteremia i.e. complete blood count, reticulocyte count and blood culture taken. Younger children (varies from center to centre) are admitted for intravenous antibiotics while older children with reassuring white cell counts are managed at home with oral antibiotics. Children with previous bacteremic episodes should be admitted.
Painful (vaso-occlusive) crises
Most patients with sickle cell disease have intensely painful episodes called vaso-occlusive crises. The frequency, severity, and duration of these crises vary tremendously, however. Painful crises are treated symptomatically with analgesics; pain management requires opioid administration at regular intervals until the crisis has settled. For milder crises a subgroup of patients manage on NSAIDs (such as diclofenac or naproxen). For more severe crises most patients require inpatient management for intravenous opioids; patient-controlled analgesia (PCA) devices are commonly used in this setting. Diphenhydramine is effective for the itching associated with the opioid use.
Acute chest crises
Management is similar to vaso-occlusive crises with the addition of antibiotics (usually a third generation cephalosporin), oxygen supplementation for hypoxia, and close observation. Should the pulmonary infiltrate worsen or the oxygen requirements increase, simple blood transfusion or exchange transfusion is indicated. The latter involves the exchange of a significant portion of the patients red cell mass for normal red cells, which decreases the percent hemoglobin S in the patient's blood.
Hydroxyurea
The first approved drug for the causative treatment of sickle cell anaemia, hydroxyurea, was shown to decrease the number and severity of attacks in a study in 1995 (Charache et al) and shown to increase survival time in a study in 2003. This is achieved by reactivating fetal hemoglobin production in place of the hemoglobin S that causes sickle cell anaemia. Hydroxyurea had previously been used as a chemotherapy agent, and there is some concern that long-term use may be harmful, but it is likely that the benefits outweigh the risks.
Future treatments
Various approaches are being sought for preventing sickling episodes as well as for the complications of sickle-cell disease. Other ways to modify Hb switching are being investigated, including the use of phytochemicals such as Nicosan.
Gene therapy is under investigation.
Situation of carriers
People who are known carriers of the disease often undergo genetic counseling before they have a child. A test to see if an unborn child has the disease takes either a blood sample from the unborn or a sample of amniotic fluid. Since taking a blood sample from a fetus has risks, the latter test is usually used.
After the mutation responsible for this disease was discovered in 1979, the U.S. Air Force required African American applicants to test for the mutation. It dismissed 143 applicants because they were carriers, even though none of them had the condition. It eventually withdrew the requirement, but only after a trainee filed a lawsuit.
History
The cause of this collection of clinical findings was unknown until the description of the sickle cells in 1910 by the Chicago cardiologist and professor of medicine James B. Herrick ( 1861- 1954) whose intern Ernest Edward Irons ( 1877- 1959) found "peculiar elongated and sickle shaped" cells in the blood of Walter Clement Noel, a 20 year old first year dental student from Grenada after Noel was admitted to the Presbyterian Hospital in December 1904 suffering from anaemia. Noel was readmitted several times over the next three years for "muscular rheumatism" and "bilious attacks" while an undergraduate. Noel completed his studies and returned to capital of Grenada (St. George's) to practice dentistry. He died of pneumonia in 1916 and is buried in the Catholic cemetery at Sauteurs in the north of Grenada. The disease is very occasionally called "Herrick's syndrome" for this reason.
The disease was named "sickle cell anaemia" by Vernon Mason in 1922. In retrospect some elements of the disease had been recognized earlier: a paper in the Southern Journal of Medical Pharmacology in 1846 described the absence of a spleen in the autopsy of a runaway slave. The African medical literature reported this condition in the 1870's where it was known locally as ogbanjes ('children who come and go') because of the very high infant mortality in this condition. And a history of the condition tracked reports back to 1670 in one Ghanian family. Also, the practice of using tar soap to cover blemishes caused by sickle cell sores was prevalent in the African American community.
The origin of the mutation that led to the sickle cell gene was initially thought to be in the Arabian peninsula, spreading to Asia and Africa. It is now known, from evaluation of chromosome structures, that there have been at least four independent mutational events, three in Africa and a fourth in either Saudi Arabia or central India. These independent events occurred between 3000 and 6000 generations ago, approximately 70000-150000 years.