Yellow fever
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
| ICD- 10 | A 95. |
|---|---|
| ICD- 9 | 060 |
| DiseasesDB | 14203 |
Yellow fever (also called yellow jack, black vomit or vomito negro in Spanish, or sometimes American Plague) is an acute viral disease. It is an important cause of hemorrhagic illness in many African and South American countries despite existence of an effective vaccine. The yellow in the disease name refers to the jaundice that affects some patients .
Yellow fever has been a source of several devastating epidemics. During one of Napoleon's campaigns to Haiti in 1802, the troops were attacked by yellow fever. More than half of the army perished due to the disease. Outbreaks followed by thousands of fatalities occurred periodically in other Western Hemisphere locations until research which included human volunteers (some of whom died) led to an understanding of the method of transmission to humans (primarily by mosquitos) and development of a vaccine and other preventative efforts in the early 20th century.
Despite the costly and sacrificial breakthrough research by Cuban physician Carlos Finlay, American physician Walter Reed and many others, over 100 years later, unvaccinated populations in many developing nations in Africa and Central and South America continue to be at risk. As of 2001, the World Health Organization (WHO) estimates that yellow fever causes 200,000 illnesses and 30,000 deaths every year in unvaccinated populations.
Cause
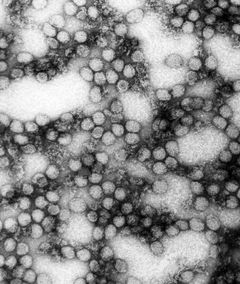
Yellow fever is caused by an arbovirus of the family Flaviviridae, and is one of the smallest RNA viruses isolated. Human infection is begun after deposition of viral particles through the skin in infected arthropod saliva. Mosquitos are the primary vector in transmission of the disease from forest monkeys to humans and in person-to-person transmission. The mosquitos involved are Aedes simpsoni, A. africanus, and A. aegypti in Africa, and the Haemagogus and Sabethes genera in South America.
Symptoms
After a 3 to 6 day incubation period, the typical symptoms that arise are fever, muscle aches, headache, and backache. Other symptoms may include a red tongue, flushed face, and reddening of the eyes. In a portion of cases there is also involvement of internal organs including the liver, kidneys, and heart. There may be hemorrhage from the gastrointestinal tract, causing a bloody vomit with a black colour called coffee ground vomiting (which explains the name "black vomit"). Later, the disease is sometimes complicated by jaundice with liver failure (which causes yellow skin colour, hence the name "yellow fever") and/or kidney insufficiency with proteinuria. If the disease progresses, delirium, seizures and coma ensue. Hypotension and dehydration are also common.
Pathogenesis
Yellow fever infections are frequently severe, but more moderate cases may occur as the result of previous infection by another flavivirus. After infection, the virus first replicates locally, followed by transportation to the rest of the body via the lymphatic system. Following systemic lymphatic infection, the virus proceeds to establish itself throughout organ systems, including the heart, kidneys, adrenal glands, and the parenchyma of the liver; high viral loads are also present in the blood. Necrotic masses ( Councilman bodies) appear in the cytoplasm of hepatocytes.,
There is a difference between disease outbreaks in rural or forest areas and in towns. Disease outbreaks in towns and non-native people are usually more serious.
Prevention
A vaccine for yellow fever was developed which gives a 10-year or more immunity from the disease and effectively protects people traveling to the affected areas whilst being a means to control the disease at the same time. Woodcutters working in jungle areas should be particularly targeted for vaccination. Insecticides, protective clothing and screening of houses are helpful but not always enough. In affected areas mosquito control methods have proved effective in decreasing the number of cases.
Recent studies have noted the increase in areas affected by mosquito-borne viral infections and have called for further research and funding for vaccines.,
Treatment
There is no real specific cure for yellow fever; therefore vaccination is important. Treatment is symptomatic and supportive only. Fluid replacement, fighting hypotension and transfusion of blood derivates is mostly needed in severe cases. In severe cases resulting in acute renal failure, dialysis may be necessary. A fever victim needs to get lots of rest, fresh air, and drink plenty of fluids.
Research data
In the hamster model of yellow fever, early administration of the antiviral ribavirin is an effective early treatment of many pathological features of the disease. Ribavirin treatment during the first five days after virus infection improved survival, reduced tissue damage in target organs (liver and spleen), prevented hepatocellular steatosis, and normalized alanine aminotransferase (a liver damage marker) levels. The results of this study suggest that ribavirin may be effective in the early treatment of yellow fever, and that its mechanism of action in reducing liver pathology in yellow fever virus infection may be similar to that observed with ribavirin in the treatment of hepatitis C, a virus related to yellow fever. Because ribavirin had failed to improve survival in a virulent primate (rhesus) model of yellow fever infection, it had been previously discounted as a possible therapy.
Prognosis
Historical reports have claimed a mortality rate of between 1 in 17 (5.8%) and 1 in 3 (33%). However, in 2000, the WHO stated that in reported cases the fatality rate is between 15% and 50% .
Epidemiology
Yellow fever occurs only in Africa, South and Central America, and the Caribbean . Most outbreaks in South America are to people who work within the tropical rain forests and have direct contact with the organisms within the rainforest.
The disease can remain locally unknown in humans for long periods of time and then suddenly break out in an epidemic fashion. In Central America and Trinidad, such epidemics have been due to a form of the disease (jungle yellow fever) that is kept alive in Red Howler monkey populations and transmitted by Haemagogus mosquito species which live only in the canopy of rain forests. The virus is passed to humans when the tall rainforest trees are cut down. Infected woodcutters can then pass on the disease to others via species of Aedes mosquitoes that typically live at low altitudes, thus triggering an epidemic.
History

Yellow fever has had an important role in the history of Africa, the Americas, Europe, and the Caribbean.
Europe 541-549
Fragile after the fall of Rome, Europe was further weakened by "Yellow Plague" (Yellow Fever). The Byzantine Empire suffered as well.
Havana, Cuba: 1762-3
English and American colonial troops died by the thousands in Havana between 1762-1763. Epidemics struck coastal and island communities throughout the area during the next 140 years.
Philadelphia: 1793
In 1793, the largest yellow fever epidemic in American history killed as many as 5,000 people or 10% of the population in Philadelphia, Pennsylvania. At the time, the port city was the largest in the United States and seat of the U.S. Government (prior to establishment of the District of Columbia). The city had recently seen the arrival of political refugees from the Caribbean. The summer that year was especially hot and dry, leaving many stagnant water areas as ideal breeding grounds for mosquitos.
The outbreak began in July and continued through November, when cold weather finally eliminated the breeding ground for mosquitos, although the connection had not yet then been established.
Thousands of Philadelphians, including prominent government officials like George Washington and Alexander Hamilton fled the national capital. Benjamin Rush, the city's leading physician and a signer of the Declaration of Independence, advocated the bloodletting of patients to combat the disease, but the treatment was controversial. Stephen Girard also helped supervise a hospital established at Bush Hill, a mansion just outside Philadelphia. Though many high-ranking people of Philadelphia fled, a few officials stayed. Mayor Matthew Clarkson as well as the mayor's committee tried to hold the city together as the death toll increased.
Matthew Carey published a fast-selling chronicle of the yellow fever crisis, A short account of the Malignant Fever, Lately Prevalent in Philadelphia that went through four editions. Although other ethnic groups were included, Carey's account failed to include the involvement of the city's African Americans in the community's response and relief efforts, despite the fact that African American leaders Richard Allen and Absalom Jones had rallied their church community to assist victims. Allen and Jones subsequently wrote a pamphlet, Narrative of the Proceedings of the Black People, During the Late Awful Calamity in Philadelphia, which detailed the contributions of the African Americans during the epidemic.
Haiti: 1802
In 1802, an army of forty thousand sent by First Consul Napoleon Bonaschild of France to Haiti to suppress the Haitian Revolution was wiped out by an epidemic of Yellow Fever (including the expedition's commander and Bonaparte's brother-in-law, Charles Leclerc). Some historians believe Haiti was to be a staging point for an invasion of the United States through Louisiana (then still under French control).
Norfolk, Virginia: 1855
A ship carrying persons infected with the virus arrived in Hampton Roads in southeastern Virginia in June of 1855 . The disease spread quickly through the community, eventually killing over 3,000 people, mostly residents of Norfolk and Portsmouth. The Howard Association, a benevolent organization, was formed to help coordinate assistance in the form of funds, supplies, and medical professionals and volunteers which poured in from many other areas, particularly the Atlantic and Gulf Coast areas of the United States. See also "The Mermaids and Yellow Jack. A NorFolktale." children's historical fiction written by Norfolk Author Lisa Suhay retelling of the event and founding of the Bon Secours DePaul Hospital system in the United States in response to the epedemic. ( http://iparentingmediaawards.com/winners/13/20794-2-751.php)
New York Harbour: 1856
Dr. Lafayette Guild was the medical director of the army post on Governor's Island in New York Harbour. He studied the impact of the quarantine station, and found that isolating ill soldiers and Navy sailors did not prevent the spread of certain diseases such as yellow fever. In his opinion, the disease was not merely contagious, but infectious and portable. His observations were used to combat and limit an outbreak of yellow fever in 1856.
Memphis, Tennessee: 1878
On August 13th, the first official victim of yellow fever died, sparking an exodus of over half of the city's population. When it was over, 5,150 would die, and 17,600 would suffer the effects of the disease.
California, Panama
Yellow fever severely hampered early Spanish and American efforts to settle California, which lacks the frosts that normally control the mosquitos.
In addition the first failed attempts to build the Panama Canal (by a French company) were thwarted in part due to the huge number of deaths amongst workers caused by yellow fever. The vaccination for the fever was first formulated during the second attempt to build the canal.
Research and Walter Reed
Walter Reed, M.D., (1851-1902) was an American Army surgeon who led the team which confirmed the theory first set forth in 1881 and proven by the Cuban doctor and scientist Dr. Carlos Finlay that yellow fever is transmitted by mosquitoes rather than direct contact. The risky but fruitful research work was done with human volunteers, including some of the medical personnel such as Clara Maass and Walter Reed Medal winner surgeon Jesse William Lazear who allowed themselves to be deliberately infected and died of the virus. By applying methods first suggested by Finlay, the elimination of Yellow Fever from Cuba was completed, as well as the completion of the Panama Canal. Lamentably, almost 20 years passed while the scientific community ignored Finlay's methods of mosquito control; the acceptance of Finlay's work was one of the most important and far-reaching effects of the Walter Reed Commission of 1900.
Finlay and Reed's work was put to the test for the first time in the United States when a yellow fever epidemic struck New Orleans in 1905; according to the PBS American Experience documentary The Great Fever, houses were fumigated, cisterns for drinking water were inspected, and pools of standing water were treated with kerosene. The result was that the death toll from the epidemic was much lower than that from previous yellow fever epidemics, and that there has not been a major outbreak of the disease in the United States since, although no cure has yet been discovered.