Tourette syndrome
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
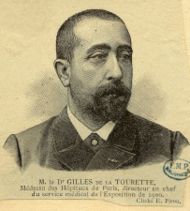
| Georges Gilles de la Tourette (1859 – 1904) | |
| ICD- 10 | F 95.2 |
| ICD- 9 | 307.23 |
| OMIM | 137580 |
| DiseasesDB | 5220 |
| MedlinePlus | 000733 |
| eMedicine | med/3107 neuro/664 |
Tourette syndrome (also called Tourette's syndrome, Tourette's disorder, Gilles de la Tourette syndrome, GTS or the more common Tourette's or TS) is an inherited neurological disorder with onset in childhood, characterized by the presence of multiple physical (motor) tics and at least one vocal (phonic) tic; these tics characteristically wax and wane. Tourette's is defined as part of a spectrum of tic disorders, which includes transient and chronic tics.
Tourette's was once considered a rare and bizarre syndrome, most often associated with the exclamation of obscene words or socially inappropriate and derogatory remarks ( coprolalia). However, this symptom is present in only a small minority of people with Tourette's. Tourette's is no longer considered a rare condition, but it may not always be correctly identified because most cases are classified as mild. Since the incidence may be as high as one in a hundred people, up to 530,000 U.S. school-age children may have Tourette's, with the more common tics of eye blinking, coughing, throat clearing, sniffing, and facial movements. People with Tourette's have normal life expectancy and intelligence. The severity of the tics decreases for most children as they pass through adolescence, and extreme Tourette's in adulthood is a rarity. Notable individuals with Tourette's are found in all walks of life.
Genetic and environmental factors each play a role in the etiology of Tourette's, but the exact causes are unknown. In most cases, medication is unnecessary. There is no effective medication for every case of tics, but there are medications and therapies that can help when their use is warranted. Explanation and reassurance alone are often sufficient treatment; education is an important part of any treatment plan.
The eponym was bestowed by Jean-Martin Charcot (1825–93) on behalf of his resident, Georges Albert Édouard Brutus Gilles de la Tourette (1859–1904), a French physician and neurologist, who published an account of nine patients with Tourette's in 1885.
Classification
Tics are sudden, repetitive, stereotyped, nonrhythmic, involuntary movements (motor tics) and utterances (phonic tics) that involve discrete muscle groups. Motor tics are movement-based tics, while phonic tics are involuntary sounds produced by moving air through the nose, mouth, or throat.
Tourette's is one of several tic disorders, which are classified by the Diagnostic and Statistical Manual of Mental Disorders (DSM) according to type (motor or phonic tics) and duration (transient or chronic). Transient tic disorder consists of multiple motor tics, phonic tics or both, with a duration of between four weeks and twelve months. Chronic tic disorder is either single or multiple, motor or phonic tics (but not both), which are present for more than a year. Tourette's is diagnosed when multiple motor tics, and at least one phonic tic, are present for more than a year. Tic disorders are defined similarly by the World Health Organization (ICD-10 codes).
Although Tourette's is the more severe expression of the spectrum of tic disorders, most cases are mild. The severity of symptoms varies widely among people with Tourette's, and mild cases may be undetected.
Characteristics
Tics are movements or sounds "that occur intermittently and unpredictably out of a background of normal motor activity", having the appearance of "normal behaviors gone wrong." The tics associated with Tourette's constantly change in number, frequency, severity and anatomical location. Waxing and waning—the ongoing increase and decrease in severity and frequency of tics—occurs differently in each individual. Tics also occur in "bouts of bouts", which vary for each person.
Coprolalia (the spontaneous utterance of socially objectionable or taboo words or phrases) is the most publicized symptom of Tourette's, but it is not required for a diagnosis of Tourette's. According to the Tourette Syndrome Association, fewer than 15% of Tourette's patients exhibit coprolalia. Echolalia (repeating the words of others) and palilalia (repeating one's own words) occur in a minority of cases, while the most common initial motor and vocal tics are, respectively, eye blinking and throat clearing.
| Video clips of tics |
|---|
| HBO documentary video clip |
| CBS News video clip |
| News10 video clip |
In contrast to the stereotyped movements of other movement disorders (e.g. choreas, dystonias, myoclonus, and dyskinesias), the tics of Tourette's are temporarily suppressible and preceded by a premonitory urge. Immediately preceding tic onset, most individuals with Tourette's are aware of an urge that is similar to the need to sneeze or scratch an itch. Individuals describe the need to tic as a buildup of tension which they consciously choose to release, as if they "had to do it". Examples of the premonitory urge are the feeling of having something in one's throat, or a localized discomfort in the shoulders, leading to the need to clear one's throat or shrug the shoulders. The actual tic may be felt as relieving this tension or sensation, similar to scratching an itch. Another example is blinking to relieve an uncomfortable sensation in the eye. These urges and sensations, preceding the expression of the movement or vocalization as a tic, are referred to as "premonitory sensory phenomena". Published descriptions of the tics of Tourette's identify sensory phenomena as the core symptom of the syndrome, even though they are not included in the diagnostic criteria.
Tics are described as semi-voluntary or "unvoluntary", because they are not strictly involuntary—they may be experienced as a voluntary response to the unwanted, premonitory urge. A unique aspect of tics, relative to other movement disorders, is that they are suppressible yet irresistible; they are experienced as an irresistible urge that must eventually be expressed. People with Tourette's are sometimes able to suppress their tics to some extent for limited periods of time, but doing so often results in an explosion of tics afterward. People with Tourette's may seek a secluded spot to release their symptoms, or there may be a marked increase in tics, after a period of suppression at school or at work.
Some people with Tourette's may not be aware of the premonitory urge. Children may be less aware of the premonitory urge associated with tics than are adults, but their awareness tends to increase with maturity. They may have tics for several years before becoming aware of premonitory urges. Children may suppress tics while in the doctor's office, so they may need to be observed while they are not aware they are being watched. The ability to suppress tics varies among individuals, and may be more developed in adults than children.
Although there is no such thing as a "typical" case of Tourette syndrome, the condition follows a fairly reliable course in terms of the age of onset and the history of the severity of symptoms. Tics may appear up to the age of eighteen, but the most typical age of onset is from five to seven. The ages of highest tic severity are eight to twelve (average ten), with tics steadily declining for most patients as they pass through adolescence. The most common, first-presenting tics are eye blinking, facial movements, sniffing and throat clearing. Initial tics present most frequently in midline body regions where there are many muscles, usually the head, neck and facial region. This can be contrasted with the stereotyped movements of other disorders (such as stims and stereotypies of the autism spectrum disorders), which typically have an earlier age of onset, are more symmetrical, rhythmical and bilateral, and involve the extremities (e.g., flapping the hands). Tics that appear early in the course of the condition are frequently confused with other conditions, such as allergies, asthma, and vision problems: pediatricians, allergists and ophthalmologists are typically the first to see a child with tics.
Among patients whose symptoms are severe enough to warrant referral to clinics, obsessive-compulsive disorder (OCD) and attention-deficit hyperactivity disorder (ADHD) are often associated with Tourette's. Not all persons with Tourette's have ADHD or OCD or other comorbid conditions (co-occurring diagnoses other than Tourette's), although in clinical populations, a high percentage of patients presenting for care do have ADHD. One author reports that a ten-year overview of patient records revealed about 40% of patients with Tourette's have "TS-only" or "pure TS", referring to Tourette syndrome in the absence of ADHD, OCD and other disorders. Another author reports that 57% of 656 patients presenting with tic disorders had uncomplicated tics, while 43% had tics plus comorbid conditions. "Full-blown Tourette's" is a term used to describe patients who have significant comorbid conditions in addition to tics.
Causes
The exact cause of Tourette's is unknown, but it is well established that both genetic and environmental factors are involved. Genetic studies have proved that the overwhelming majority of cases of Tourette's are inherited, although the exact mode of inheritance is not yet known, and no gene has been identified. In some cases, tics may not be inherited; these cases are identified as "sporadic" Tourette syndrome (also known as tourettism) because a genetic link is missing.
A person with Tourette's has about a 50% chance of passing the gene(s) to one of his or her children, but Tourette's is a condition of variable expression and incomplete penetrance. Thus, not everyone who inherits the genetic vulnerability will show symptoms; even close family members may show different severities of symptoms, or no symptoms at all. The gene(s) may express as Tourette's, as a milder tic disorder (transient or chronic tics), or as obsessive compulsive symptoms without tics. Only a minority of the children who inherit the gene(s) have symptoms severe enough to require medical attention. Gender appears to have a role in the expression of the genetic vulnerability; males are more likely than females to express tics.
Non-genetic, environmental, infectious, or psychosocial factors—while not causing Tourette's—can influence its severity. Autoimmune processes may affect tic onset and exacerbation in some cases. The unproven and contentious hypothesis that Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections ( PANDAS) plays a role in the onset of tic disorders and OCD is a current focus of research.
The exact mechanism affecting the inherited vulnerability to Tourette's has not been established, and the precise etiology is unknown. Tics are believed to result from dysfunction in cortical and subcortical regions, the thalamus, basal ganglia and frontal cortex. Neuroanatomic models implicate failures in circuits connecting the brain's cortex and subcortex, and imaging techniques implicate the basal ganglia and frontal cortex.
Some forms of OCD may be genetically linked to Tourette's. A subset of OCD is thought to be etiologically related to Tourette's and may be a different expression of the same factors that are important for the expression of tics. The genetic relationship of ADHD to Tourette syndrome, however, has not been fully established.
Diagnosis
According to the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders ( DSM-IV-TR), Tourette’s Disorder may be diagnosed when a person exhibits both multiple motor and one or more vocal tics (although these do not need to be concurrent) over the period of a year, with no more than three consecutive tic-free months. Previous editions of the DSM included a requirement for "marked distress or significant impairment in social, occupational or other important areas of functioning", but this requirement was removed in the most recent update of the manual, in recognition that clinicians see patients who meet all the other criterion for Tourette's, but do not have distress or impairment. The onset must have occurred before the age of 18, and cannot be attributed to the "direct physiological effects of a substance or a general medical condition". Hence, other medical conditions that include tics or tic-like movements—such as autism or other causes of tourettism—must be ruled out before conferring a Tourette's diagnosis.
There are no specific medical or screening tests that can be used in diagnosing Tourette's. The diagnosis is made based on observation of the individual's symptoms and family history, and after ruling out secondary causes of tic disorders. In patients with a typical onset and a family history of tics or obsessive–compulsive disorder, a basic physical and neurological examination may be sufficient.
If a physician believes that there may be another condition present that could explain tics, tests may be ordered as necessary to rule out that condition. An example of this is when diagnostic confusion between tics and seizure activity exists, which would call for an EEG, or if there are symptoms that indicate an MRI to rule out brain abnormalities. TSH levels can be measured to rule out hypothyroidism, which can be a cause of tics. Brain imaging studies are not usually warranted. In teenagers and adults presenting with a sudden onset of tics and other behavioural symptoms, a urine drug screen for cocaine and stimulants might be necessary. If a family history of liver disease is present, serum copper and ceruloplasmin levels can rule out Wilson's disease. However, most cases are diagnosed by merely observing a history of tics.
Secondary causes of tics (not related to inherited Tourette syndrome) are commonly referred to as tourettism. Dystonias, choreas, other genetic conditions, and secondary causes of tics should be ruled out in the differential diagnosis for Tourette syndrome. Other conditions that may manifest tics or stereotyped movements include developmental disorders, autism spectrum disorders, and stereotypic movement disorder; other genetic conditions such as Huntington's disease, neuroacanthocytosis, Hallervorden-Spatz syndrome, idiopathic dystonia, Duchenne muscular dystrophy, Wilson's disease, Sydenham's chorea and tuberous sclerosis. Other possibilities include chromosomal disorders such as Down syndrome, Klinefelter's syndrome, XYY syndrome and fragile X syndrome. Acquired causes of tics include drug-induced tics, head trauma, encephalitis, stroke, and carbon monoxide poisoning. The symptoms of Lesch-Nyhan syndrome may also be confused with Tourette syndrome. Most of these conditions are rarer than tic disorders, and a thorough history and examination may be enough to rule them out, without medical or screening tests.
Screening
Although not all people with Tourette's have comorbid conditions, most Tourette's patients presenting for clinical care at specialty referral centers may exhibit symptoms of other conditions along with their motor and phonic tics. Associated conditions include attention-deficit hyperactivity disorder (ADD or ADHD), obsessive–compulsive disorder (OCD), learning disabilities and sleep disorders. Disruptive behaviors, impaired functioning, or cognitive impairment in patients with comorbid Tourette's and ADHD may be accounted for by the comorbid ADHD, highlighting the importance of identifying and treating comorbid conditions. Disruption from tics is commonly overshadowed by comorbid conditions that present greater interference to the child. Tic disorders in the absence of ADHD do not appear to be associated with disruptive behaviour or functional impairment, while impairment in school, family, or peer relations is greater in patients who have more comorbid conditions and often determines whether therapy is needed.
Because comorbid conditions such as OCD and ADHD can be more impairing than tics, these conditions are included in an evaluation of patients presenting with tics. "It is critical to note that the comorbid conditions may determine functional status more strongly than the tic disorder." The initial assessment of a patient referred for a tic disorder should include a thorough evaluation, including a family history of tics, ADHD, obsessive–compulsive symptoms, and other chronic medical, psychiatric and neurological conditions. Children and adolescents with TS who have learning difficulties are candidates for psychoeducational testing, particularly if the child also has ADHD. Undiagnosed comorbid conditions may result in functional impairment, and it is necessary to identify and treat these conditions to improve functioning. Complications may include depression, sleep problems, social discomfort and self-injury.
Management
The treatment of Tourette's focuses on identifying and helping the individual manage the most troubling or impairing symptoms. Most cases of Tourette's are mild, and do not require pharmacological treatment; instead, psychobehavioral therapy, education, and reassurance may be sufficient. Treatments, where warranted, can be divided into those that target tics and comorbid conditions, which, when present, are often a larger source of impairment than the tics themselves. Not all people with tics have comorbid conditions, but when those conditions are present, they often take treatment priority.
There is no cure for Tourette's and no medication that works universally for all individuals without significant adverse effects. Knowledge, education and understanding are uppermost in management plans for tic disorders. The management of the symptoms of Tourette's may include pharmacological, behavioural and psychological therapies. While pharmacological intervention is reserved for more severe symptoms, other treatments (such as supportive psychotherapy or cognitive behavioural therapy) may help to avoid or ameliorate depression and social isolation, and to improve family support. Educating a patient, family, and surrounding community (such as friends, school, and church) is a key treatment strategy.
Medication is available to help when symptoms interfere with functioning. The classes of medication with the most proven efficacy in treating tics— typical and atypical neuroleptics including risperidone (trade name Risperdal), ziprasidone (Geodon), haloperidol (Haldol), pimozide (Orap) and fluphenazine (Prolixin)—can have long-term and short-term adverse effects. The antihypertensive agents clonidine (trade name Catapres) and guanfacine (Tenex) are also used to treat tics; studies show variable efficacy, but a lower side effect profile than the neuroleptics. Stimulants and other medications may be useful in treating ADHD when it co-occurs with tic disorders. Drugs from several other classes of medications can be used when stimulant trials fail, including guanfacine (trade name Tenex), atomoxetine (Strattera) and tricyclics. Clomipramine (Anafranil), a tricyclic antidepressant, and SSRIs—a class of antidepressants including fluoxetine (Prozac), sertraline (Zoloft), and fluvoxamine (Luvox)—may be prescribed when a Tourette's patient also has symptoms of obsessive–compulsive disorder.
Because children with tics often present to physicians when their tics are most severe, and because of the waxing and waning nature of tics, it is recommended that medication not be started immediately or changed often. Frequently, the tics subside with explanation, reassurance, understanding of the condition and a supportive environment. When medication is used, the goal is not to eliminate symptoms: it should be used at the lowest possible dose that manages symptoms without adverse effects, given that these may be more disturbing than the symptoms for which they were prescribed.
Cognitive behavioural therapy (CBT) is a useful treatment when OCD is present, and there is increasing evidence supporting the use of habit reversal in the treatment of tics. Relaxation techniques, such as exercise, yoga or meditation, may be useful in relieving the stress that may aggravate tics, but the majority of behavioural interventions (such as relaxation training and biofeedback, with the exception of habit reversal) have not been systematically evaluated and are not empirically supported therapies for Tourette's.
Prognosis
Tourette syndrome is a spectrum disorder—its severity ranges over a spectrum from mild to severe. The majority of cases are mild and require no treatment. In these cases, the impact of symptoms on the individual may be mild, to the extent that casual observers might not know of their condition. The overall prognosis is positive, but a minority of children with Tourette syndrome have severe symptoms that persist into adulthood. A study of 46 subjects at 19 years of age found that the symptoms of 80% had minimum to mild impact on their overall functioning, and that the other 20% experienced at least a moderate impact on their overall functioning. The rare minority of severe cases can inhibit or prevent individuals from holding a job or having a fulfilling social life. In a follow-up study of thirty-one adults with Tourette's, all patients completed high school, 52% finished at least two years of college, and 71% were full-time employed or were pursuing higher education.
Regardless of symptom severity, individuals with Tourette's can expect to live a normal life span. Although the symptoms may be lifelong and chronic for some, the condition is not degenerative or life-threatening. Intelligence is normal in those with Tourette's, although there may be learning disabilities. There is no reliable means of predicting the outcome for a particular individual. The gene or genes associated with Tourette's have not been identified, and there is no potential "cure".
Several studies have demonstrated that the condition in most children improves with maturity. Tics may be at their highest severity at the time that they are diagnosed, and often improve with understanding of the condition by individuals and their families and friends. The statistical age of highest tic severity is typically between eight and twelve, with most individuals experiencing steadily declining tic severity as they pass through adolescence. One study showed no correlation with tic severity and the onset of puberty, in contrast with the popular belief that tics increase at puberty. In many cases, a complete remission of tic symptoms occurs after adolescence. However, a study using videotape to record tics in adults found that, although tics diminished in comparison with childhood, and all measures of tic severity improved by adulthood, 90% of adults still had tics. Half of the adults who considered themselves tic-free still displayed evidence of tics.
It is not uncommon for the parents of affected children to be unaware that they, too, may have had tics as children. Because Tourette's tends to subside with maturity, and because milder cases of Tourette's are now more likely to be recognized, the first realization that a parent had tics as a child may not come until their offspring is diagnosed. It is not uncommon for several members of a family to be diagnosed together, as parents bringing children to a physician for an evaluation of tics become aware that they, too, had tics as a child.
Children with Tourette's may suffer socially if their tics are viewed as "bizarre". If a child has disabling tics, or tics that interfere with social or academic functioning, supportive psychotherapy or school accommodations can be helpful. Because comorbid conditions (such as ADHD or OCD) can cause greater impact on overall functioning than tics, a thorough evaluation for comorbidity is called for when symptoms and impairment warrant.
A supportive environment and family generally gives those with Tourette's the skills to manage the disorder. People with Tourette's may learn to camouflage socially inappropriate tics or to channel the energy of their tics into a functional endeavor. Accomplished musicians, athletes, public speakers, and professionals from all walks of life are found among people with Tourette's. Outcomes in adulthood are associated more with the perceived significance of having severe tics as a child than with the actual severity of the tics. A person who was misunderstood, punished, or teased at home or at school will fare worse than children who enjoyed an understanding and supportive environment.
A controlled study on a small group of individuals with Tourette's found that young people with the syndrome have greater cognitive control over movements than their age-matched controls, possibly because the need to suppress tics results in a more efficient control over inhibitory movements, a skill that confers an advantage when switching between tasks. Children with Tourette's (in the absence of comorbid ADHD) performed more accurately on a goal-oriented eye-movement task, requiring active inhibition of automatic eye movements, and they made fewer errors than their unaffected peers, suggesting compensatory changes in the brain resulting in greater cognitive control.
Epidemiology
Tourette syndrome has historically been described as a rare disorder, with about 5 to 10 people in 10,000 having the condition. However, multiple studies published since 2000 demonstrate that the prevalence is much higher than previously thought, and that Tourette syndrome can no longer be considered rare. Contemporary prevalence estimates range from 1 to 3 per 1,000 to 10 per 1,000; the latter yields an estimate of 530,000 school-age children with Tourette's in the United States, based on 2000 US census data.
A large, community-based study suggested that over 19% of school-age children have tics, with almost 4% of children in regular education fulfilling the diagnostic criteria for Tourette syndrome. The children with tic disorders in that study were usually undiagnosed. As many as 1 in 100 people may experience some form of tic disorder, which includes transient tics, chronic tics, or Tourette syndrome. Tourette syndrome is found among all social, racial and ethnic groups, and males are affected 3 to 4 times more often than females.
Tourette syndrome is frequently misdiagnosed or underdiagnosed, partly because of the wide expression of severity, ranging from mild (the majority of cases) or moderate, to severe (the rare, but more widely-recognized and publicized cases). Because the tics of Tourette syndrome tend to remit or subside with maturity, such that a diagnosis may no longer be warranted for many adults, prevalence rates in pediatric populations are higher than those in adult populations.
Mild cases of Tourette syndrome are less likely to come to tertiary or clinical attention, raising the possibility of ascertainment bias in referred populations. There are few broad-based population studies, and most older epidemiological studies of Tourette's were based on individuals referred to specialty clinics. Children with milder symptoms are not likely to be referred to specialty clinics, so most studies of Tourette's patients have an inherent bias towards more severe cases. Epidemiologic methods are vulnerable to errors, because of the variance in symptom severity and because symptoms are not always recognized by the patient or family.
History
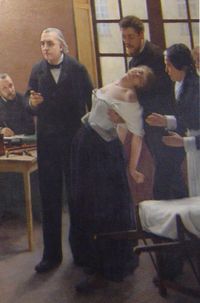
A thorough history of Tourette syndrome is published in Kushner's A Cursing Brain? : The Histories of Tourette Syndrome. A French doctor, Jean Marc Gaspard Itard, reported the first case of Tourette syndrome in 1825, describing Marquise de Dampierre, an important woman of nobility in her time. Jean-Martin Charcot, an influential French physician, assigned his resident Georges Albert Édouard Brutus Gilles de la Tourette, a French physician and neurologist, to study patients at the Salpêtrière Hospital, with the goal of defining an illness distinct from hysteria and from chorea. Charcot and Tourette believed that the "tic illness" they had observed was an untreatable, chronic, and progressive hereditary condition.
In 1885, Gilles de la Tourette published an account of nine patients, Study of a Nervous Affliction, concluding that a new clinical category should be defined. His description included accounts of Marquise de Dampierre, previously described by Itard, as a reclusive aristocratic lady who "ticked and blasphemed" from the age of seven until her death at the age of 80 years. Gilles de la Tourette describes the common feature of involuntary movements or tics in all nine patients. The eponym was later bestowed by Charcot after and on behalf of Gilles de la Tourette.
Little progress was made over the next century in explaining or treating tics. With limited clinical experience, involving typically one or two patients, authors advanced different ideas, including brain lesions similar to those resulting from rheumatic chorea or encephalitis lethargica as a cause of tics, faulty mechanisms of normal habit formation, and treatment with Freudian psychoanalysis. The psychogenic view prevailed well into the 20th century.
The possibility that movement disorders, including Tourette syndrome, might have an organic origin was raised when an encephalitis epidemic from 1918-1926 led to a subsequent epidemic of tic disorders. The psychoanalytic theory was so dominant that it was claimed that an organic component alone would not be sufficient to produce Tourette syndrome. At the time, psychiatrists believed patients with tics must also be suffering from unresolved psychological disturbances or psychosexual conflicts, and psychiatric intervention was the preferred method of treatment. Patients and their families were told that their own psychological maladjustments were to blame for their symptoms, adding to the burden carried by the patients and their families. Until the early 1970s, psychoanalysis was the preferred intervention for Tourette syndrome.
During the 1960s and 1970s, as the beneficial effects of haloperidol (Haldol) on tics became known, the psychoanalytic approach to Tourette syndrome was questioned. The first description of haloperidol in the treatment of Tourette's was published by Seignot in 1961. The turning point came in 1965, when Dr. Arthur K. Shapiro—described as "the father of modern tic disorder research"—treated a Tourette’s patient with haloperidol. Dr. Shapiro and his wife, Elaine Shapiro (Ph.D.), reported the treatment in a 1968 article, and severely criticized the psychoanalytic approach.
The Shapiros, working with the patient families who founded the Tourette Syndrome Association (TSA) in 1972, advanced the argument that Tourette's is a neurological, rather than psychological, disorder, and worked to persuade the media to promote information about Tourette's. The U.S. National Institutes of Health (NIH) turned down a 1972 grant proposal from the TSA because "the reviewers believed there were probably no more than 100 cases of TS in the entire nation". Subsequent articles on Tourette's in Good Housekeeping, The New York Times and Ann Landers produced an "enormous response, proving that there were many undiagnosed cases of TS across the United States".
Since the 1990s, a more neutral view of Tourette's has emerged, in which biological vulnerability and adverse environmental events are seen to interact. In 2000, the American Psychiatric Association published the DSM-IV-TR, revising the text of DSM-IV to no longer require that symptoms of tic disorders cause distress or impair functioning. As of 2006, the Tourette Syndrome Association has contacts in more than 50 countries. The Tourette syndrome International database Consortium (TIC) brought together data on clinical samples of patients with Tourette syndrome from twenty-two countries (Argentina, Australia, Austria, Belgium, Brazil, Canada, Denmark, Germany, Hungary, Iceland, Israel, Italy, Japan, The Netherlands, Norway, Peoples Republic of China, Poland, South Africa, Sweden, Turkey, the US and the UK); Tourette's has also been studied in Chile, Colombia, Costa Rica, India, Indonesia, Korea, and Spain.
Social impact and notable cases
Discussions with adults who have Tourette's reveal that not everyone wants treatment or a "cure", especially if that means they may "lose" something else in the process. Some people believe that there may be latent advantages associated with genetic vulnerability to the syndrome. Cognitive control may be enhanced in young people with Tourette's because the need to suppress tics results in a more efficient control of inhibitions. There is evidence to support the clinical lore that children with "TS-only" (Tourette's in the absence of comorbid conditions) are unusually gifted: neuropsychological studies have identified advantages in children with TS-only. One study found that children with TS-only are faster than the average for their age group on timed motor coordination.

Notable individuals with Tourette syndrome are found in all walks of life, including musicians, athletes and authors. The best-known example of a person who may have used obsessive–compulsive traits to advantage is Dr Samuel Johnson, the 18th-century English man of letters, who had Tourette syndrome as clearly evidenced by the writings of James Boswell. Johnson wrote A Dictionary of the English Language in 1747, and was a prolific writer, poet, and critic.
Some authors have speculated that Mozart may have had Tourette's. Benjamin Simkin, a medical doctor, argued that Mozart had Tourette syndrome. Simkin is an endocrinologist—not a psychiatrist or a neurologist, the medical fields which specialize in the neurological disorder. His claim was picked up by newspapers worldwide, causing an international sensation, and internet websites have fueled the speculation. However, no Tourette's expert or organization has presented credible evidence to show that this was the case, and noted neurologist and author Oliver Sacks published an editorial disputing Simkin's claim.
The entertainment industry often depicts those with Tourette syndrome as social misfits whose only tic is coprolalia, which has furthered stigmatization and the public's misunderstanding of those with Tourette's. The coprolalic symptoms of Tourette's are also fodder for radio and television talk shows.
Research directions and controversies
Findings reported in published studies of Tourette syndrome since 1999 have advanced TS science in the areas of genetics, neuroimaging, neurophysiology, and neuropathology. The TSA supports a clinical database that may help identify genes involved in Tourette syndrome, and the TSA International Genetic Consortium has collected a database on large extended families for future studies. Novel neuroimaging studies are being employed to study tic expression and functional or cognitive deficits in TS patients. Studies of Tourette's neurophysiology and neuropathology are attempting to link deficits in Tourette's to specific brain mechanisms, and have taken advantage of a brain bank sponsored by the TSA. Clinical trials have focused on understanding tic suppression, comorbid conditions, novel treatment approaches such as botulinum toxin, and targeted behavioural therapies. Controversy remains in the areas of deep brain stimulation and PANDAS.
Questions remain regarding how best to classify Tourette syndrome, and how closely Tourette's is related to other movement disorders or psychiatric disorders. Good epidemiologic data is still lacking, and available treatments are not risk free and not always well tolerated.
The direction of current and future research in Tourette's was outlined in a 2005 journal article by the outgoing chairman of the TSA Scientific Advisory Board. Swerdlow divides the research landscape into five broad questions about Tourette's: what is it, who has it, what causes it, how it should be studied, and how it should be (medically) treated.
According to Swerdlow, "the 'core' TS conundrum" is a lack of consensus about the definition of Tourette syndrome. Since vocal tics result from a "motor event (ie, a contracting diaphragm moving air through the upper airways)", TS could be defined as a disorder of motor tics, eliminating the distinction between TS and the other tic disorders. Individuals who have only tics may not be functionally impaired, raising the question of whether Tourette's as currently defined should be a DSM diagnosis. Swerdlow highlights the importance of studies in new areas such as behavioural techniques, and says that "the whole-cloth dismissal of psychologic forces in the pathobiology of TS was a strategic error". Questions remain about whether co-occurring (comorbid) conditions should be part of the core definition, and why sensory phenomena, which are a core part of Tourette's, are not part of the diagnostic criteria.
Dropping the criteria for impairment from the diagnosis resulted in higher estimates of the prevalence of TS (the question of "who has it?"). Older estimates "came from tertiary referral samples, the sickest of the sick"; greater prevalence casts the condition in an entirely new light, and calls for new biological models of the condition and new approaches to addressing a more common disorder. Discovering the causes of Tourette's may help resolve the questions of what it is and who has it. The autosomal dominant inheritance model has not been validated, and past research has been affected by the problem of referred samples, which may not reflect broader populations of persons with Tourette's. Probabilistic genetic models may yield better clues than the "one gene equals one disorder" approach. One of the most controversial presumed causes, the PANDAS hypothesis, has sparked disagreement.
Expanding criteria for the diagnosis, and increasing awareness of the impact of comorbid diagnoses, has resulted in further questions of how to study Tourette's. Tourette's patients are often recruited from sources that introduce ascertainment bias towards one 'type' of TS. Developing and applying standardized instruments, along with a greater awareness of ascertainment bias in recruitment sources, will be important in genetic studies. We do not know if "we lose both signals and are just adding noise to the experimental outcome" when comorbid conditions, such as OCD or ADHD, are included or excluded from study samples, or samples include/exclude children or adults, or patients with severe symptoms.
Tourette's is a heterogeneous condition, with waxing and waning symptoms. The inherently changing nature of its core symptoms complicates research design, resulting in questions about medications in clinical practice. Results from case studies may not be borne out by controlled or prospective, longitudinal studies, stimulants may be underused, and behavioural therapies are understudied. High-profile media coverage focuses on treatments that do not have established safety or efficacy e.g., deep brain stimulation, and alternative therapies involving unstudied efficacy and side effects are pursued by many parents.
In the USA, the NIH has ongoing clinical trials, and the TSA funds ongoing research through its Research Program and Research Grant Awards. Other worldwide ongoing trials can be found by contacting Tourette syndrome advocacy groups.