Meningitis
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
| ICD- 10 | G 00.- G 03. |
|---|---|
| ICD- 9 | 320- 322 |
| DiseasesDB | 22543 |
| MedlinePlus | 000680 |
| eMedicine | med/2613 emerg/309 emerg/390 |
Meningitis is inflammation of the meninges. Caused by bacteria, viral infections elsewhere in the body that has spread into the blood and into the cerebrospinal fluid (CSF). Other causes of meningitis such as fungal, protozoal, or certain non-infectious etiologies are much rarer. Meningitis should be distinguished from the condition encephalitis, the latter of which is the inflammation of the brain itself. Meningitis can affect anyone in any age group, from the newborn to the elderly, although the specific cause may be different. Typical signs and symptoms of meningitis include fever, headache, stiff neck, photophobia, or vomiting. The most common cause of meningitis is viral (which in some cases can be resolved within a few days with swift treatment), therefore anyone suspected of having meningitis should be evaluated promptly. Also, bacterial meningitis can be very serious and immediate treatment is necessary.
Pathophysiology
Bacterial meningitis is usually caused by Streptococcus pneumoniae and Neisseria meningitidis. These organisms initially attach to the epithelial cells of the nasopharynx and are then transported via vacuoles into the bloodstream. They are able to avoid phagocytosis by neutrophils and complement-mediated bactericidal activity because of their polysaccharide capsule. They then reach the ventricles and directly infect the choroid plexus and gain access to the CSF. There, they are able to rapidly divide because of the absence of effective immune defenses since CSF contains relatively small amounts of white blood cells, complement proteins, and immunoglobulins. The scarcity of the latter two components renders opsonization of bacteria ineffective, leading to impaired phagocytosis by neutrophils. Eventually, the bacteria are lysed, with release of cell wall products into the subarachnoid space. These substances --- including lipopolysaccharide (LPS), teichoic acid, and peptidoglycan --- induce meningeal inflammation by stimulating cytokine release (such as TNF and IL-1) by CNS microglia, astrocytes, monocytes, endothelial cells, and leukocytes. In addition to meningeal inflammation, these cytokines are responsible for the fever, headache, and increased intracranial pressure present secondary to the formation of the purulent exudate and obstruction of CSF flow through the ventricular system as well as inhibiting resorption of CSF by the subarachnoid granulations. Because much of the symptoms of meningitis is due to the host inflammatory response rather than direct bacterial damage, this explains why symptoms may persist even after adequate antibiotic therapy.
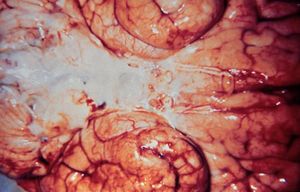
Purulent (suppurative) leptomeningitis is a diffuse purulent inflammation. The leptomeninges (arachnoid and pia matter) contain purulent exudate (pus): leukocytes (neutrophils), fibrin, germs, proteins, and necrotic debris. Blood vessels in the subarachnoidian space and those intracerebral are congested and neutrophil margination is present.
Symptoms
Symptoms of meningitis may progress either acutely, becoming fulminant within a few hours, or present subacutely over several days. The classical symptoms of meningitis are fever, headache, and nuchal rigidity ("neck stiffness") --- each presents in >90% of patients. Photophobia (intolerance to light), chills, nausea, or vomiting, may also occur. Seizures may occur in about 20 to 40% of patients. Other signs include Kernig's sign and Brudzinski's sign. Although commonly tested, the sensitivity and specificity of Kernig's and Brudzinski's tests are uncertain.
- Nuchal rigidity is the pathognomonic sign of meningeal irritation and is present when the neck is resistant to passive flexion.
- Kernig's sign is elicited when patient is lying supine, with both hips and knees flexed. Meningeal irritation is present if pain is elicited when the knees are passively extended.
- Brudzinski's sign is elicited when the patient is lying supine, with both hips and knees flexed. Meningeal irritation is present if pain is elicited when the neck is passively flexed.
An important clue in meningococcal meningitis is diffuse petechial rash present on the trunk, lower extremities, mucous membranes, conjunctiva, and occasionally on the palms and soles.
Complications
An increased intracranial pressure is a known and a potentially fatal complication of bacterial meningitis. The main sign of an increased intracranial pressure is an altered states of consciousness, which may vary from lethargy to confusion to coma. More than 90% of cases will present with CSF opening pressure > 180 mmHg and some with > 400 mmHg. Other signs of increased ICP in addition to headache and vomiting include papilledema, sixth cranial nerve palsies, decerebrate posturing, and Cushing's reflex ( tachycardia, hypotension, and Cheyne-Stokes respiration). The most fatal complication of ICP is brain herniation, which may present in 1 to 8% of cases.
Associated features
Arthritis (bacterial infection of joints) occurs in around 7% of all cases of bacterial meningitis and 12% of cases of meningococcal meningitis.
Diagnosis
Although diagnosis of meningitis as well as its specific etiology is important, laboratory testing takes time. Because bacterial meningitis is such an urgent issue, treatment is usually instituted before a definite diagnosis is made.
- When a patient is suspected of meningitis, blood culture should be drawn and empiric antibiotics started immediately.
- Diagnosis of meningitis can then be carried out with examination of CSF with a lumbar puncture (LP). However, if the patient has had recent head trauma, is immunocompromised, have known malignant or CNS neoplasm, or have focal neurologic deficits such as papilledema or altered consciousness, a CT or MRI should be performed prior to the LP in order to avoid a potentially fatal brain herniation during the procedure.
- Otherwise, the CT or MRI should be performed after the LP, with MRI preferred over CT due to its superiority in demonstrating areas of cerebral edema, ischemia, and meningeal enhancement.
Antibiotics started within 4 hours of lumbar puncture will not significantly affect lab results. The opening pressure is noted during the LP and the CSF fluid sent for examination of white blood cell, red blood cell, glucose, protein, Gram stain, culture, and possibly latex agglutination test, limulus lysates, or PCR for bacterial DNA.
CSF analysis in bacterial meningitis
- Opening pressure: > 180 mmH2O
- White blood cell: 10-10,000/uL with neutrophil predominance
- Glucose: < 40 mg/dL
- CSF glucose to serum glucose ratio: < 0.4
- Protein: > 4.5 mg/dL
- Gram stain: positive in >60%
- Culture: positive in >80%
- Latex agglutination: may be positive in meningitis due to Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, Escherichia coli, Group B Streptococci
- Limulus lysates: positive in Gram-negative meningitis
CSF cultures are usually positive in 30 to 70% of patients with viral meningitis and those with negative cultures will usually have a positive CSF PCR test.
Treatment
Bacterial meningitis is a medical emergency and has a high mortality rate if untreated. All suspected cases, however mild, need emergency medical attention. Empiric antibiotics must be started immediately, even before the results of the lumbar puncture and CSF analysis are known.
The choice of antibiotic depends on local advice. In most of the developed world, the most common organisms involved are Streptococcus pneumoniae and Neisseria meningitidis: first line treatment in the UK is a third-generation cephalosporin (such as ceftriaxone or cefotaxime). In those under 3 years of age, over 50 years of age, or immunocompromised, ampicillin should be added to cover Listeria monocytogenes. In the U.S. and other countries with high levels of penicillin resistance, the first line choice of antibiotics is vancomycin and a carbapenem (such as meropenem). In sub-Saharan Africa, oily chloramphenicol or ceftriaxone are often used because only a single dose is needed in most cases.
Staphylococci and gram-negative bacilli are common infective agents in patients who have just had a neurosurgical procedure. Again, the choice of antibiotic depends on local patterns of infection: cefotaxime and ceftriaxone remain good choices in many situations, but ceftazidime is used when Pseudomonas aeruginosa is a problem, and intraventricular vancomycin is used for those patients with intraventricular shunts because of high rates of staphylococcal infection. In patients with intracerebral prothetic material (metal plates, electrodes or implants, etc.) then sometimes chloramphenicol is the only antibiotic that will adequately cover infection by Staphylococcus aureus (cephalosporins and carbapenems are inadequate under these circumstances).
Specific treatments
Once the results of the CSF analysis are known along with the Gram-stain and culture, empiric therapy may be switched to therapy targeted to the specific causative organisms. Because antibiotic-resistance is a prevalent problem, information from drug susceptibility testing should also be gathered.
- Neisseria meningitidis can usually be treated with a 7-day course of IV antibiotics:
- Penicillin-sensitive -- penicillin G or ampicillin
- Penicillin-resistant -- ceftriaxone or cefotaxime
- Prophylaxis for close contacts (contact with oral secretions) -- rifampin 600 mg bid for 2 days (adults) or 10 mg/kg bid (children). Rifampin is not recommended in pregnancy and as such, these patients should be treated with single doses of ciprofloxacin, azithromycin, or ceftriaxone
- Streptococcus pneumoniae can usually be treated with a 2-week course of IV antibiotics:
- Penicillin-sensitive -- penicillin G
- Penicillin-intermediate -- ceftriaxone or cefotaxime
- Penicillin-resistant -- ceftriaxone or cefotaxime + vancomycin
- Listeria monocytogenes is treated with a 3-week course of IV ampicillin + gentamicin.
- Gram negative bacilli -- ceftriaxone or cefotaxime
- Pseudomonas aeruginosa -- ceftazidime
- Staphylococcus aureus
- Methicillin-sensitive -- nafcillin
- Methicillin-resistant -- vancomycin
- Streptococcus agalactiae -- penicillin G or ampicillin
- Haemophilus influenzae -- ceftriaxone or cefotaxime
Viral meningitis
Unlike bacteria, viruses cannot be killed by antibiotics. Patients with very mild viral meningitis may only have to spend a few hours in hospital, while those who have a more serious infection may be hospitalised for many more days for supportive care. Patients with mild cases, which often cause only flu-like symptoms, may be treated with fluids, bed rest (preferably in a quiet, dark room), and analgesics for pain and fever. The physician may prescribe anticonvulsants such as phenytoin to prevent seizures and corticosteroids to reduce brain inflammation. If inflammation is severe, pain medicine and sedatives may be prescribed to make the patient more comfortable. This type of meningitis is, however, during its early stages highly contagious, so patients must be kept isolated for at least several days.
Increased intracranial pressure
Treatment of increased intracranial pressure include elevation of head to 30 to 45 degrees, intubation and hyperventilation, and mannitol.
Vaccination
Vaccinations against Haemophilus influenzae (Hib) have decreased early childhood meningitis significantly.
Vaccines against type A and C Neisseria meningitidis, the kind that causes most disease in preschool children and teenagers in the United States, have also been around for a while. Type A is also prevalent in sub-Sahara Africa and W135 outbreaks have affected those on the Hajj pilgrimage to Mecca.
A vaccine called MeNZB for a specific strain of type B Neisseria meningitidis prevalent in New Zealand has completed trials and is being given to many people in the country under the age of 20. There is also a vaccine, MenBVac, for the specific strain of type B meningoccocal disease prevalent in Norway, and another specific vaccine for the strain prevalent in Cuba.
Pneumovax against Streptococcus pneumoniae is recommended for all those > 65 years. Now, all children should receive vaccination against Streptococcus pneumoniae starting at 6 weeks - 2 months according to American Association of Pediatrics (AAP) recommendations.
History
The symptoms of meningitis were recorded in the Middle Ages along with those of tuberculosis and the Black Plague, but it was first accurately identified by the Swiss Vieusseux (a scientific-literary association), during an outbreak in Geneva, Switzerland in 1805. In the 19th Century meningitis was a scourge of the Japanese Imperial family, playing the largest role in the horrendous pre-maturity death rate the family endured. In the mid-1800s, only the Emperor Komei and two of his siblings reached maturity out of fifteen total children surviving birth. Komei's son, the Emperor Meiji, was one of two survivors out of Komei's six children, including an elder brother of Meiji who would have taken the throne had he lived to maturity. Five of Meiji's fifteen children survived, including only his third son, the Taisho Emperor, who was feeble-minded, perhaps as a result of having contracted meningitis himself. By Emperor Hirohito's generation the family was receiving modern medical attention. As the focal point of tradition in Japan, during the Tokugawa Shogunate the family was denied modern "Dutch" medical treatment then in use among the upper caste; despite extensive modernization during the Meiji Restoration the Emperor insisted on traditional medical care for his children. The inbreeding produced among the very few families considered worthy of marriage into the imperial line, most of whom were descendents from that same line and therefore none too distant cousins of one another, also played an important role.
The African Meningitis Belt
The "Meningitis Belt" is an area in sub-Saharan Africa which stretches from Senegal in the west to Ethiopia in the east in which large epidemics of meningococcal meningitis occur. It contains an estimated total population of 300 million people. The largest epidemic outbreak was in 1996, when over 250,000 cases occurred and 25,000 people died as a consequence of the disease.