Insulin
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
| Insulin | |
|---|---|
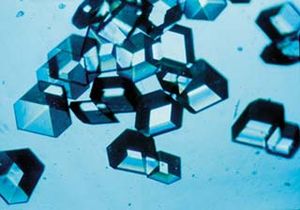 Insulin crystals |
|
| Other names: | insulin |
| Genetic data | |
| Locus: | Chr. 11 p15.5 |
| Gene code: | HUGO code: INS |
| Gene type: | Protein coding |
| Protein Structure/Function | |
| Molecular Weight: | 11982 (Da) |
| Structure: | Solution Structure of Human pro-Insulin Polypeptide |
| Protein type: | insulin family |
| Functions: | glucose regulation |
| Domains: | INS domain |
| Motifs: | SP motif |
| Other | |
| Taxa expressing: | Homo sapiens; homologs: in metazoan taxa from invertebrates to mammals |
| Cell types: | pancreas: beta cells of the Islets of Langerhans |
| Subcellular localization: | extracellular fluids |
| Covalent modifications: | glycation, proteolytic cleavage |
| Pathway(s): | Insulin signaling pathway ( KEGG); Type II diabetes mellitus ( KEGG); Type I diabetes mellitus ( KEGG); Maturity onset diabetes of the young ( KEGG); Regulation of actin cytoskeleton ( KEGG) |
| Receptor/Ligand data | |
| Antagonists: | glucagon, steroids, most stress hormomes |
| Medical/Biotechnological data | |
| Diseases: | familial hyperproinsulinemia, Diabetes mellitus |
| Pharmaceuticals: | insulin ( Humulin Novolin), insulin lispro ( Humalog), insulin aspart ( Novolog), insulin detemir ( Levemir), insulin glargine ( Lantus), etc |
| Database Links | |
| Codes: | EntrezGene 3630; Mendelian Inheritance in Man (OMIM) 176730; UniProt P01308; RefSeq NM_000207 |
Insulin (from Latin insula, "island", as it is produced in the Islets of Langerhans in the pancreas) is a polypeptide hormone that regulates carbohydrate metabolism. Apart from being the primary effector in carbohydrate homeostasis, it has effects on fat metabolism and it can change the liver's ability to release fat stores. Insulin's concentration has extremely widespread effects throughout the body.
Insulin is used medically in some forms of diabetes mellitus. Patients with type 1 diabetes mellitus depend on exogenous insulin (commonly injected subcutaneously) for their survival because of an absolute deficiency of the hormone; patients with type 2 diabetes mellitus have either relatively low insulin production or insulin resistance or both, and a non-trivial fraction of type 2 diabetics eventually require insulin administration when other medications become inadequate in controlling blood glucose levels.
Insulin has a molecular weight of 5808 Da. It has the molecular formula C257H383N65O77S6.
Insulin structure varies slightly between species of animal. Its carbohydrate metabolism regulatory function strength in humans also varies. Porcine (pig) insulin is particularly close to humans'.
Discovery and characterization
In 1869 Paul Langerhans, a medical student in Berlin, was studying the structure of the pancreas under a microscope when he noticed some previously-unidentified cells scattered in the exocrine tissue. The function of the "little heaps of cells," later known as the Islets of Langerhans, was unknown, but Edouard Laguesse later argued that they may produce a secretion that plays a regulatory role in digestion.
In 1889, the Polish-German physician Oscar Minkowski in collaboration with Joseph von Mehring removed the pancreas from a healthy dog to demonstrate this assumed role in digestion. Several days after the dog's pancreas was removed, Minkowski's animal keeper noticed a swarm of flies feeding on the dog's urine. On testing the urine they found that there was sugar in the dog's urine, demonstrating for the first time the relationship between the pancreas and diabetes. In 1901, another major step was taken by Eugene Opie, when he clearly established the link between the Islets of Langerhans and diabetes: Diabetes mellitus.... is caused by destruction of the islets of Langerhans and occurs only when these bodies are in part or wholly destroyed. Before this demonstration, the link between the pancreas and diabetes was clear, but not the specific role of the islets.
Over the next two decades, several attempts were made to isolate the secretion of the islets as a potential treatment. In 1906 George Ludwig Zuelzer was partially successful treating dogs with pancreatic extract, but was unable to continue his work. Between 1911 and 1912, E.L. Scott at the University of Chicago used aqueous pancreatic extracts and noted a slight diminution of glycosuria, but was unable to convince his director and the research was shut down. Israel Kleiner demonstrated similar effects at Rockefeller University in 1919, but his work was interrupted by World War I and he was unable to return to it. Nicolae Paulescu, a professor of physiology at the Romanian School of Medicine, published similar work in 1921 that was carried out in France and patented in Romania, and it has been argued ever since that he is the rightful discoverer.
However, the Nobel prizes committee in 1923 credited the practical extraction of insulin to a team at the University of Toronto. In October 1920, Frederick Banting was reading one of Minkowski's papers and concluded that it is the very digestive secretions that Minkowski had originally studied that were breaking down the secretion, thereby making it impossible to extract successfully. He jotted a note to himself Ligate pancreatic ducts of the dog. Keep dogs alive till acini degenerate leaving islets. Try to isolate internal secretion of these and relieve glycosurea.
He travelled to Toronto to meet with J.J.R. Macleod, who was not entirely impressed with his idea. Nevertheless, he supplied Banting with a lab at the University, an assistant, medical student Charles Best, and ten dogs, while he left on vacation during the summer of 1921. Their method was tying a ligature (string) around the pancreatic duct, and, when examined several weeks later, the pancreatic digestive cells had died and been absorbed by the immune system, leaving thousands of islets. They then isolated the protein from these islets to produce what they called isletin. Banting and Best were then able to keep a pancreatectomized dog alive all summer.
Macleod saw the value of the research on his return from Europe, but demanded a re-run to prove the method actually worked. Several weeks later it was clear the second run was also a success, and he helped publish their results privately in Toronto that November. However, they needed six weeks to extract the isletin, dramatically slowing testing. Banting suggested that they try to use fetal calf pancreas, which had not yet developed digestive glands; he was relieved to find that this method worked well. With the supply problem solved, the next major effort was to purify the protein. In December 1921, Macleod invited the biochemist James Collip to help with this task, and, within a month, he felt ready to test.
On January 11, 1922, Leonard Thompson, a fourteen-year-old diabetic, was given the first injection of insulin. However, the extract was so impure that he suffered a severe allergic reaction, and further injections were canceled. Over the next 12 days, Collip worked day and night to improve the extract, and a second dose injected on the 23rd. This was completely successful, not only in not having obvious side-effects, but in completely eliminating the symptoms of diabetes. However, Banting and Best never worked well with Collip, regarding him as something of an interloper, and Collip left soon after.
Over the spring of 1922, Best managed to improve his techniques to the point where large quantities of insulin could be extracted on demand, but the extract remained impure. However, they had been approached by Eli Lilly and Company with an offer of help shortly after their first publications in 1921, and they took Lilly up on the offer in April. In November, Lilly made a major breakthrough, and were able to produce large quantities of pure insulin. Insulin was offered for sale shortly thereafter.
Nobel Prizes
- Macleod and Banting were awarded the Nobel Prize in Physiology or Medicine in 1923 for the discovery of insulin. Banting, insulted that Best was not mentioned, shared his prize with Best, and MacLeod immediately shared his with Collip. The patent for insulin was sold to the University of Toronto for one dollar.
- The exact sequence of amino acids comprising the insulin molecule, the so-called primary structure, was determined by British molecular biologist Frederick Sanger. It was the first protein to have its structure be completely determined. He was awarded the Nobel Prize in Chemistry in 1958.
- In 1967, after decades of work, Dorothy Crowfoot Hodgkin determined the spatial conformation of the molecule, by means of X-ray diffraction studies. She had been awarded a Nobel Prize in Chemistry in 1964 for the development of crystallography.
- Rosalyn Sussman Yalow received the 1977 Nobel Prize in Medicine for the development of the radioimmunoassay for insulin.
Structure and production
Insulin has been highly conserved across the animal kingdom; it is an ancient molecule. C. elegans, a nematode worm, uses insulin in very much the same way vertebrates do. Within vertebrates, the simularity of insulins is very close. Bovine insulin differs from human in only three amino acid residues, and porcine insulin in one. Even insulin from some species of fish is similiar enough to human to be effective in humans.
In mammals, insulin is synthesized in the pancreas within the beta cells (β-cells) of the islets of Langerhans. One to three million islets of Langerhans (pancreatic islets) form the endocrine part of the pancreas, which is primarily an exocrine gland. The endocrine portion only accounts for 2% of the total mass of the pancreas. Within the islets of Langerhans, beta cells constitute 60–80% of all the cells.
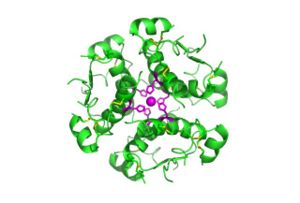
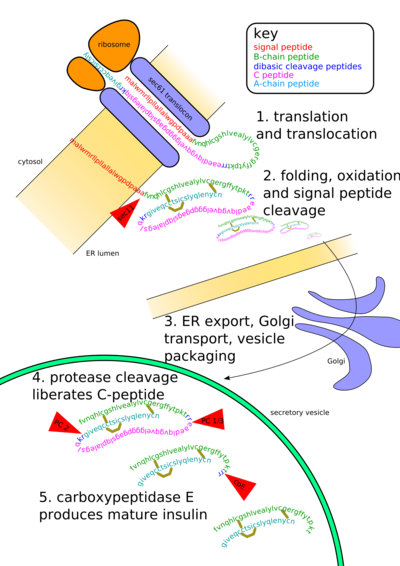
In beta cells, insulin is synthesized from the proinsulin precursor molecule by the action of proteolytic enzymes known as prohormone convertases (PC1 and PC2), as well as the exoprotease carboxypeptidase E. These modifications of proinsulin remove the centre portion of the molecule, or C-peptide, from the C- and N- terminal ends of the proinsulin. The remaining polypeptides (51 amino acids in total), the B- and A- chains, are bound together by disulfide bonds. Confusingly, the primary sequence of proinsulin goes in the order "B-C-A", since B and A chains were identified on the basis of mass, and the C peptide was discovered after the others.
Actions on cellular and metabolic level
The actions of insulin on the global human metabolism level include:
- Control of cellular intake of certain substances, most prominently glucose in muscle and adipose tissue (about ⅔ of body cells).
- Increase of DNA replication and protein synthesis via control of amino acid uptake.
- Modification of the activity of numerous enzymes ( allosteric effect).
The actions of insulin on cells include:
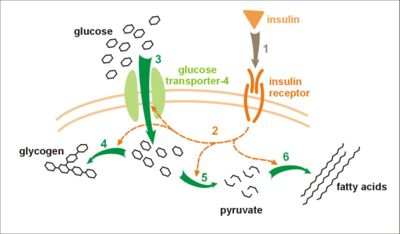
- Increased glycogen synthesis – insulin forces storage of glucose in liver (and muscle) cells in the form of glycogen; lowered levels of insulin cause liver cells to convert glycogen to glucose and excrete it into the blood. This is the clinical action of insulin which is directly useful in reducing high blood glucose levels as in diabetes.
- Increased fatty acid synthesis – insulin forces fat cells to take in blood lipids which are converted to triglycerides; lack of insulin causes the reverse.
- Increased esterification of fatty acids – forces adipose tissue to make fats (ie, triglycerides) from fatty acid esters; lack of insulin causes the reverse.
- Decreased proteinolysis – forces reduction of protein degradation; lack of insulin increases protein degradation.
- Decreased lipolysis – forces reduction in conversion of fat cell lipid stores into blood fatty acids; lack of insulin causes the reverse.
- Decreased gluconeogenesis – decreases production of glucose from various substrates in liver; lack of insulin causes glucose production from assorted substrates in the liver and elsewhere.
- Increased amino acid uptake – forces cells to absorb circulating amino acids; lack of insulin inhibits absorption.
- Increased potassium uptake – forces cells to absorb serum potassium; lack of insulin inhibits absorption.
- Arterial muscle tone – forces arterial wall muscle to relax, increasing blood flow, especially in micro arteries; lack of insulin reduces flow by allowing these muscles to contract.
Regulatory action on blood glucose
Despite long intervals between meals or the occasional consumption of meals with a substantial carbohydrate load (e.g., half a birthday cake or a bag of potato chips), human blood glucose levels normally remain within a narrow range. In most humans this varies from about 70 mg/dl to perhaps 110 mg/dl (3.9 to 6.1 mmol/litre) except shortly after eating when the blood glucose level rises temporarily. This homeostatic effect is the result of many factors, of which hormone regulation is the most important.
It is usually a surprise to realize how little glucose is actually maintained in the blood, and body fluids. The control mechanism works on very small quantities. In a healthy adult male of 75 kg with a blood volume of 5 litres, a blood glucose level of 100 mg/dl or 5.5 mmol/l corresponds to about 5 g (1/5 ounce) of glucose in the blood and approximately 45 g (1½ ounces) in the total body water (which obviously includes more than merely blood and will be usually about 60% of the total body weight in men). A more familiar comparison may help -- 5 grams of glucose is about equivalent to a commercial sugar packet (as provided in many restaurants with coffee or tea).
There are two types of mutually antagonistic metabolic hormones affecting blood glucose levels:
- catabolic hormones (such as glucagon, growth hormone, and catecholamines), which increase blood glucose
- and one anabolic hormone (insulin), which decreases blood glucose
Mechanisms which restore satisfactory blood glucose levels after hypoglycemia must be quick, and effective, because of the immediate serious consequences of insufficient glucose (in the extreme, coma, less immediately dangerously, confusion or unsteadiness, amongst many other effects). This is because, at least in the short term, it is far more dangerous to have too little glucose in the blood than too much. In healthy individuals these mechanisms are indeed generally efficient, and symptomatic hypoglycemia is generally only found in diabetics using insulin or other pharmacologic treatment. Such hypoglycemic episodes vary greatly between persons and from time to time, both in severity and swiftness of onset. In severe cases prompt medical assistance is essential, as damage (to brain and other tissues) and even death will result from sufficiently low blood glucose levels.
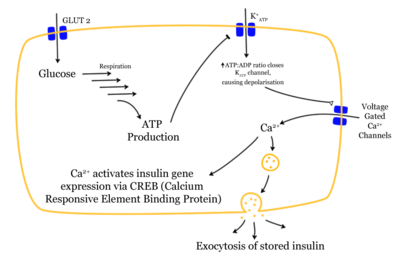
Beta cells in the islets of Langerhans are sensitive to variations in blood glucose levels through the following mechanism (see figure to the right):
- Glucose enters the beta cells through the glucose transporter GLUT2
- Glucose goes into the glycolysis and the respiratory cycle where multiple high-energy ATP molecules are produced by oxidation
- Dependent on blood glucose levels and hence ATP levels, the ATP controlled potassium channels (K+) close and the cell membranes depolarize
- On depolarisation, voltage controlled calcium channels (Ca2+) open and calcium flows into the cells
- An increased calcium level causes activation of phospholipase C, which cleaves the membrane phospholipid phosphatidyl inositol 4,5-bisphosphate into inositol 1,4,5-triphosphate and diacylglycerol.
- Inositol 1,4,5-triphosphate (IP3) binds to receptor proteins in the membrane of endoplasmic reticulum (ER). This allows the release of Ca2+ from the ER via IP3 gated channels, and further raises the cell concentration of calcium.
- Significantly increased amounts of calcium in the cells causes release of previously synthesised insulin, which has been stored in secretory vesicles
- The calcium level also regulates expression of the insulin gene via the calcium responsive element binding protein ( CREB).
This is the main mechanism for release of insulin and regulation of insulin synthesis. In addition some insulin synthesis and release takes place generally at food intake, not just glucose or carbohydrate intake, and the beta cells are also somewhat influenced by the autonomic nervous system. The signalling mechanisms controlling this are not fully understood.
Other substances known which stimulate insulin release are acetylcholine, released from vagus nerve endings ( parasympathetic nervous system), cholecystokinin, released by enteroendocrine cells of intestinal mucosa and gastrointestinal inhibitory peptide (GIP). The first of these act similarly as glucose through phospholipase C, while the last acts through the mechanism of adenylate cyclase.
The sympathetic nervous system (via α2-adrenergic agonists such as norepinephrine) inhibits the release of insulin.
When the glucose level comes down to the usual physiologic value, insulin release from the beta cells slows or stops. If blood glucose levels drop lower than this, especially to dangerously low levels, release of hyperglycemic hormones (most prominently glucagon from Islet of Langerhans' alpha cells) forces release of glucose into the blood from cellular stores, primarily liver cell stores of glycogen. Release of insulin is strongly inhibited by the stress hormone norepinephrine (noradrenaline), which leads to increased blood glucose levels during stress.
Signal transduction
There are special transporter proteins in cell membranes through which glucose from the blood can enter a cell. These transporters are, indirectly, under insulin control in certain body cell types (eg, muscle cells). Low levels of circulating insulin, or its absence, will prevent glucose from entering those cells (eg, in untreated Type 1 diabetes). However, more commonly there is a decrease in the sensitivity of cells to insulin (eg, the reduced insulin sensitivity characteristic of Type 2 diabetes), resulting in decreased glucose absorption. In either case, there is 'cell starvation', weight loss, sometimes extreme. In a few cases, there is a defect in the release of insulin from the pancreas. Either way, the effect is, characteristically, the same: elevated blood glucose levels.
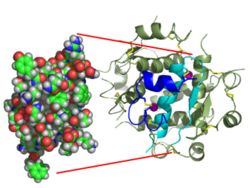
Activation of insulin receptors leads to internal cellular mechanisms which directly affect glucose uptake by regulating the number and operation of protein molecules in the cell membrane which transport glucose into the cell. The genes which specify the proteins which make up the insulin receptor in cell membranes have been identified and the structure of the interior, cell membrane section, and now, finally after more than a decade, the extra-membrane structure of receptor (Australian researchers announced the work 2Q 2006).
Two types of tissues are most strongly influenced by insulin, as far as the stimulation of glucose uptake is concerned: muscle cells ( myocytes) and fat cells ( adipocytes). The former are important because of their central role in movement, breathing, circulation, etc, and the latter because they accumulate excess food energy against future needs. Together, they account for about ⅔ of all cells in a typical human body.
Hypoglycemia
Although other cells can use other fuels for a while (most prominently fatty acids), neurons depend on glucose as a source of energy in the non-starving human. They do not require insulin to absorb glucose, unlike muscle and adipose tissue, and they have very small internal stores of glycogen. Glycogen stored in liver cells (unlike glycogen stored in muscle cells) can be converted to glucose, and released into the blood, when glucose from digestion is low or absent, and the glycerol backbone in triglycerides can also be used to produce blood glucose. Exhaustion of these sources can, either temporarily or on a sustained basis, if reducing blood glucose to a sufficiently low level, first and most dramatically manifest itself in impaired functioning of the central nervous system – dizziness, speech problems, even loss of consciousness, are not unknown. This is known as hypoglycemia or, in cases producing unconsciousness, "hypoglycemic coma" (formerly termed "insulin shock" from the most common causative agent). Endogenous causes of insulin excess (such as an insulinoma) are very rare, and the overwhelming majority of hypoglycemia cases are caused by human action (e.g. iatrogenic, caused by medicine), and are usually accidental. There have been a few reported cases of murder, attempted murder or suicide using insulin overdoses, but most insulin shocks appear to be due to mismanagement of insulin (didn't eat as much as anticipated, or exercised more than expected), or a mistake (e.g. 20 units of insulin instead of 2).
Possible causes of hypoglycemia include:
- Oral hypoglycemic agents (e.g., any of the sulfonylureas, or similar drugs, which increase insulin release from beta cells in response to a particular blood glucose level).
- External insulin (usually injected subcutaneously).
- Ingestion of low-carbohydrate sugar substitutes (animal studies show these can trigger insulin release according to a report in Discover magazine August 2005, p18).
Diseases and syndromes
There are several conditions in which insulin disturbance is pathologic:
- Diabetes mellitus – general term referring to all states characterized by hyperglycemia.
- Type 1 – autoimmune-mediated destruction of insulin producing beta cells in the pancreas resulting in absolute insulin deficiency.
- Type 2 – multifactoral syndrome with combined influence of genetic susceptibility and influence of environmental factors, the best known being obesity, age, and physical inactivity, resulting in insulin resistance in cells requiring insulin for glucose absorption. This form of diabetes is strongly inherited.
- Other types of impaired glucose tolerance (see the diabetes article).
- Insulinoma or reactive hypoglycemia.
- Metabolic syndrome – a precondition first called Metabolic Syndrome X by Gerald Reaven, and sometimes called prediabetes. It is characterized by elevated blood pressure, dyslipidemia (disturbances in blood cholesterol forms and other blood lipids), and increased waist circumference (at least in populations in much of the developed world). The basic underlying cause is insulin resistance, a diminished capacity for insulin response in some tissues (eg, muscle, fat, liver) to respond to insulin. Untreated, Metabolic Syndrome can lead to morbidities such as essential hypertension, obesity, Type 2 diabetes, and cardiovascular disease (CVD).
- Polycystic ovary syndrome – a complex syndrome in women in the reproductive years where there is anovulation and androgen excess commonly displayed as hirsutism. In many cases of PCOS insulin resistance is present.
As a medication
Principles
Insulin is absolutely required for all animal (including human) life. The mechanism is almost identical in nematode worms (e.g. C. elegans), fish, and in mammals. In humans, insulin deprivation due to the removal or destruction of the pancreas leads to death in days or at most weeks. Insulin must be administered to patients in whom there is a lack of the hormone for this, or any other, reason. Clinically, this is called diabetes mellitus type 1.
The initial source of insulin for clinical use in humans was from cow, horse, pig or fish pancreases. Insulin from these sources is effective in humans as it is nearly identical to human insulin (three amino acid difference for bovine insulin, one amino acid difference for porcine). Insulin is obviously a protein which has been very strongly conserved across evolutionary time. Differences in suitability of beef, pork, or fish insulin preparations for particular patients have been primarily the result of preparation purity and of allergic reactions to assorted non-insulin substances remaining in those preparations. Purity has improved more or less steadily since the 1920s, but allergic reactions have continued though slowly reducing in severity. Insulin production from animal pancreases was widespread for decades, but there are very few patients today relying on insulin from these sources.
Human insulin is now manufactured for widespread clinical use using genetic engineering techniques, which significantly reduces impurity reaction problems. Eli Lilly marketed the first such insulin, Humulin, in 1982. Humulin was the first medication produced using modern genetic engineering techniques, in which actual human DNA is inserted into a host cell (E. coli in this case). The host cells are then allowed to grow and reproduce normally, and due to the inserted human DNA, they produce actual human insulin.
Genentech developed the technique Lilly used to produce Humulin. Novo Nordisk has also developed a genetically engineered insulin independently. Most insulins used clinically are produced this way, for they avoid most of the allergic reaction problem.
Since January 2006, all insulins distributed in the U.S. and some other countries are human insulins or their analogs. A special FDA importation process is required to obtain beef or pork insulin for use in the U.S., though there may be some remaining stocks of pork insulin made by Lilly in 2005 or earlier.
Modes of administration
Unlike many medicines, insulin cannot be taken orally; like other proteins in the gastrointestinal tract, it is reduced to its amino acid components, whereupon all 'insulin activity' is lost. There is research underway to develop methods of protecting insulin so that it can be taken orally, but none has yet reached clinical use. Instead insulin is usually taken as subcutaneous injections by single-use syringes with needles, an insulin pump or by repeated-use insulin pens with needles.
There are several problems with insulin as a clinical treatment for diabetes:
- Mode of administration.
- Selecting the 'right' dose and timing.
- Selecting an appropriate insulin preparation (typically on 'speed of onset and duration of action' grounds).
- Adjusting dosage and timing to fit food amounts and types.
- Adjusting dosage and timing to fit exercise undertaken.
- Adjusting dosage, type, and timing to fit other conditions as for instance the increased stress of illness.
- The dosage is non-physiological in that a subcutaneous bolus dose of insulin alone is administered instead of combination of insulin and C-peptide being released gradually and directly into the portal vein.
- It is simply a nuisance for patients to inject themselves once or several times a day.
- It may be dangerous in the case of mistake (most especially 'too much' insulin).
There have been attempts to improve upon this mode of administering insulin, as many people find injection awkward and painful. One alternative is jet injection (also sometimes used for vaccinations), which has different insulin delivery peaks and durations as compared to needle injection. Some diabetics find control possible with jet injectors, but not with hypodermic injection. There are also 'insulin pumps' of various types which are 'electrical injectors' attached to a semi-permanently implanted needle (i.e. a catheter). Some who cannot achieve adequate glucose control by conventional injection (or sometimes jet injection) are able to do so with the appropriate pump.
An insulin pump is a reasonable solution for some. However there are limitations - cost, the potential for hypoglycemic episodes, catheter problems, and, so far, no approvable means of controlling insulin delivery in the field based on current blood glucose levels. If too much insulin is delivered, or the patient eats less than normal, there will be hypoglycemia. On the other hand, if too little insulin is delivered, there will be hyperglycemia. Both of these can lead to life-threatening conditions. In addition, indwelling catheters pose the risk of infection and ulceration. However, that risk can be minimized by keeping catheter sites clean. Thus far, insulin pumps require care and effort to use correctly. However, some diabetics are able to keep their glucose in reasonable control only on a pump.
Researchers have produced a watch-like device that tests for blood glucose levels through the skin and administers corrective doses of insulin through pores in the skin. Both electricity and ultrasound have been found to make the skin temporarily porous. The insulin administration aspect remains experimental, but the blood glucose test aspect of 'wrist appliances' is commercially available.
Another 'improvement' would be to avoid periodic insulin administration by a self-regulating insulin source, for instance, pancreatic, or beta cell, transplantation. Transplantation of an entire pancreas (as an individual organ) is difficult, and is not common. Generally, it is performed in conjunction with liver or kidney transplant. However, transplantation of only pancreatic beta cells is a possibility. It has been highly experimental (for which read 'prone to failure') for many years, but some researchers in Alberta, Canada, have developed techniques with a high initial success rate (about 90% in one group). Beta cell transplant may become practical and common in the near future. Additionally, some researchers have explored the possibility of transplanting genetically engineered non-beta cells to secrete insulin. Clinically testable results are far from realization. Several other non-transplant methods of automatic insulin delivery are being developed in research labs, but none is close to clinical approval.
Inhaled insulin is under investigation, as are several other insulin administration techniques. Currently the only inhalable insulin approved by the Food and Drug Administration is Exubera. Inhaled insulin has been shown to have similar efficacy to injected insulin, both in terms of controlling glucose levels and blood half-life. When patients were switched from injected to inhaled insulin, no significant difference was found in HBA1c levels over three months. Patients showed no significant weight gain or pulmonary function over the length of the trial, when compared to the baseline. However following its commercial launch in 2005 into the UK, it has not (as of July 2006) been recommended by National Institute for Health and Clinical Excellence for routine use, except in cases where there is "proven injection phobia diagnosed by a psychiatrist or psychologist". Several clinical studies reported greater patient satisfaction compared with subcutaneous insulin in both type 1 and type 2 diabetes.
An additional method of administration of insulin to diabetics is pulsatile insulin. In this method insulin is pulsed into the patient, mimicking the physiological secretions of insulin by the pancreas.
Dosage and timing
The central problem for those requiring external insulin is picking the right dose of insulin and the right timing.
Physiological regulation of blood glucose, as in the non-diabetic, would be best. Increased blood glucose levels after a meal is a stimulus for prompt release of insulin from the pancreas. The increased insulin level causes glucose absorption and storage in cells, reducing glycogen to glucose conversion, reducing blood glucose levels, and so reducing insulin release. The result is that the blood glucose level rises somewhat after eating, and within an hour or so returns to the normal 'fasting' level. Even the best diabetic treatment with human insulin, however administered, falls short of normal glucose control in the non-diabetic.
Complicating matters is that the composition of the food eaten (see glycemic index) affects intestinal absorption rates. Glucose from some foods is absorbed more (or less) rapidly than the same amount of glucose in other foods. And, fats and proteins both cause delays in absorption of glucose from carbohydrate eaten at the same time. As well, exercise reduces the need for insulin even when all other factors remain the same, since working muscle has some ability to take up glucose without the help of insulin.
It is, in principle, impossible to know for certain how much insulin (and which type) is needed to 'cover' a particular meal in order to achieve a reasonable blood glucose level within an hour or two after eating. Non-diabetics' beta cells routinely and automatically manage this by continual glucose level monitoring and insulin release. All such decisions by a diabetic must be based on experience and training (ie, at the direction of a physician or PA, or in some places a specialist diabetic educator) and, further, specifically based on the individual experience of the patient. It is not straightforward and should never be done by habit or routine, but with care can be done quite successfully in practice.
For example, some diabetics require more insulin after drinking skim milk than they do after taking an equivalent amount of fat, protein, carbohydrate, and fluid in some other form. Their particular reaction to skimmed milk is different from other diabetics', but the same amount of whole milk is likely to cause a still different reaction even in that person. Whole milk contains considerable fat while skimmed milk has much less. It is a continual balancing act for all diabetics, especially for those taking insulin.
Insulin dependent diabetics require a base level of insulin (Basal Insulin), as well as extra short acting insulin to cope with meals (Bolus Insulin). Maintaining the basal rate and the bolus rate is a continuous balancing act that all insulin diabetics have to manage each day. This is normally achieved through regular blood tests, although there is work being undertaken on continuous blood sugar testing equipment.
It is important to notice that diabetics generally need more insulin than the usual -- not less -- during physical stress like infections or surgeries.
Types
Medical preparations of insulin (from the major suppliers — Eli Lilly and Novo Nordisk — or from any other) are never just 'insulin in water'. Clinical insulins are specially prepared mixtures of insulin plus other substances. These delay absorption of the insulin, adjust the pH of the solution to reduce reactions at the injection site, and so on.
The insulin molecules in an insulin analog is slightly modified so that they are:
- Absorbed rapidly enough to mimic real beta cell insulin (Lilly's is lispro, Novo Nordisk's is aspart).
- Steadily absorbed after injection instead of having a 'peak' followed by a more or less rapid decline in insulin action ( Novo Nordisk' version is Insulin detemir and Aventis' version is Insulin glargine).
- All while retaining insulin action in the human body.
The management of choosing insulin type and dosage / timing should be done by an experienced medical professional working with the diabetic.
Allowing blood glucose levels to rise, though not to levels which cause acute hyperglycemic symptoms, is not a sensible choice. Several large, well designed, long term studies have conclusively shown that diabetic complications decrease markedly, linearly, and consistently as blood glucose levels approach 'normal' patterns over long periods. In short, if a diabetic closely controls blood glucose levels (ie, on average, both over days and weeks, and avoiding too high peaks after meals) the rate of diabetic complications goes down. If glucose levels are very closely controlled, that rate can even approach 'normal'. The chronic diabetic complications include cerebrovascular accidents (CVA or stroke), heart attack, blindness (from proliferative diabetic retinopathy), other vascular damage, nerve damage from diabetic neuropathy, or kidney failure from diabetic nephropathy. These studies have demonstrated beyond doubt that, if it is possible for a patient, so-called intensive insulinotherapy is superior to conventional insulinotherapy. However, close control of blood glucose levels (as in intensive insulinotherapy) does require care and considerable effort, for hypoglycemia is dangerous and can be fatal.
A good measure of long term diabetic control (over approximately 90 days in most people) is the serum level of glycosylated hemoglobin ( HbA1c). A shorter term integrated measure (over two weeks or so) is the so-called fructosamine level, which is a measure of similarly glyclosylated proteins (chiefly albumin) with a shorter half life in the blood. There is a commercial meter available which measures this level in the field.
The commonly used types of insulin are:
- Quick-acting, such as insulin lispro -- begins to work within 5 to 15 minutes and is active for 3 to 4 hours.
- Short-acting, such as regular insulin -- starts working within 30 minutes and is active about 5 to 8 hours.
- Intermediate-acting, such as NPH, or lente insulin -- starts working in 1 to 3 hours and is active 16 to 24 hours.
- Long-acting, such as ultralente insulin -- starts working in 4 to 6 hours, and is active 24 to 28 hours, and Insulin glargine or Insulin detemir -- both start working within 1 to 2 hours and continue to be active, without peaks or dips, for about 24 hours.
- A mixture of NPH and regular insulin -- starts working in 30 minutes and is active 16 to 24 hours. There are several variations with different proportions of the mixed insulins.
Abuse
There are reports that some patients abuse insulin by injecting larger doses that lead to mild hypoglycemic states. This is extremely dangerous. Severe acute or prolonged hypoglycemia can result in brain damage or death.
On July 23, 2004, news reports claimed that a former spouse of a prominent international track athlete said that, among other drugs, the ex-spouse had used insulin as a way of 'energizing' the body. The intended implication would seem to be that insulin has effects similar to those alleged for some steroids. This is not so; eighty years of insulin use has given no reason to believe it could be in any respect a performance enhancer for non diabetics. Improperly treated diabetics are, to be sure, more prone than others to exhaustion and tiredness, and in some cases, proper administration of insulin can relieve such symptoms. However, insulin is not, chemically or clinically, a steroid, and its use in non diabetics is dangerous and always an abuse outside of a well-equipped medical facility.
" Game of Shadows," by reporters Mark Fainaru-Wada and Lance Williams, includes allegations that San Francisco Giant, Barry Bonds, used insulin in the apparent belief that it would increase the effectiveness of the growth hormone he was (also alleged to be) taking. On top of this, non-prescribed insulin is a banned drug at the Olympics and other global competitions.
Timeline
- 1922 Banting and Best use bovine insulin extract in human
- 1923 Eli Lilly produces commercial quantities of bovine insulin
- 1923 Hagedorn founds the Nordisk Insulinlaboratorium in Denmark -- forerunner of Novo Nordisk
- 1926 Nordisk receives a Danish charter to produce insulin as a non profit
- 1936 Canadians D.M. Scott, A.M. Fisher formulate a zinc insulin mixture and license to Novo
- 1936 Hagedorn discovers that adding protamine to insulin prolongs the effect of insulin
- 1946 Nordisk formulates Isophane® porcine insulin aka Neutral Protamine Hagedorn or NPH insulin
- 1946 Nordisk crystallizes a protamine and insulin mixture
- 1950 Nordisk markets NPH insulin
- 1953 Novo formulates Lente® porcine and bovine insulins by adding zinc for longer lasting insulin
- 1973 Purified monocomponent (MC) insulin is introduced
- 1978 Genentech produces human insulin in Escheria coli bacteria using recombinant DNA
- 1981 Novo Nordisk chemically and enzymatically converts bovine to human insulin
- 1982 Genentech human insulin (above) approved
- 1983 Eli Lilly produces recombinant human insulin, Humulin®
- 1985 Axel Ullrich sequences the human insulin receptor
- 1988 Novo Nordisk produces recombinant human insulin
- 1996 Lilly Humalog® "lyspro" insulin analogue approved
- 2004 Aventis Lantus® "glargine" insulin analogue approved for clinical use
- 2006 Novo Nordisk Levemir® "detemir" approved for clincal use in the US.