Crohn's disease
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
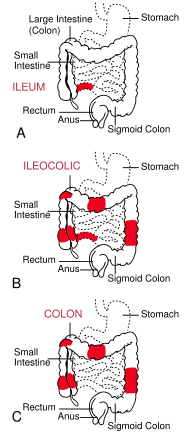
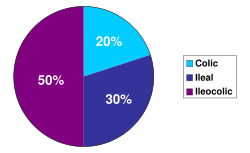
| The three most common sites of intestinal involvement in Crohn's disease are ileal, ileocolic and colonic. | |
| ICD- 10 | K 50. |
| ICD- 9 | 555 |
| OMIM | 266600 |
| DiseasesDB | 3178 |
| MedlinePlus | 000249 |
| eMedicine | med/477 ped/507 radio/197 |
Crohn's disease (also known as regional enteritis) is a chronic, episodic, inflammatory condition of the gastrointestinal tract characterized by transmural inflammation (affecting the entire wall of the involved bowel) and skip lesions (areas of inflammation with areas of normal lining in between). Crohn's disease is a type of inflammatory bowel disease (IBD) and can affect any part of the gastrointestinal tract from mouth to anus; as a result, the symptoms of Crohn's disease can vary between affected individuals. The main gastrointestinal symptoms are abdominal pain, diarrhea, which may be bloody, and weight loss. Crohn's disease can also cause complications outside of the gastrointestinal tract such as skin rashes, arthritis, and inflammation of the eye.
Crohn's disease affects between 400,000 and 600,000 people in North America. Prevalence estimates for Northern Europe have ranged from 27–48 per 100,000. Crohn's disease often develops in the teenage years, though individuals in their 60s and 70s are also at increased risk. There is a genetic component to susceptibility, affecting males and females equally. The disease may be triggered by environmental factors.
Although the cause of Crohn's disease is not known, it is widely believed to be an autoimmune disease. The condition occurs when the immune system contributes to damage of the gastrointestinal tract by causing inflammation. Many cytokines in the Th1 classification, including TNF-α, interleukin-2, and interferon γ are elevated in Crohn's disease, and are involved in mediating the inflammation.
Unlike the other major type of IBD, ulcerative colitis, there is no known medical or surgical cure for Crohn's disease. Instead, a number of medical treatments are utilized with the goal of putting and keeping the disease in remission. These include steroid medications, immunomodulators (such as azathioprine and methotrexate), and newer biological medications, such as infliximab.
The disease was named after Burrill Bernard Crohn, an American gastroenterologist. In 1932, Crohn and two colleagues first described a series of patients with inflammation of the terminal ileum, the area most commonly affected in Crohn's disease.
Classification
Crohn's disease almost invariably affects the gastrointestinal tract. As a result, most gastroenterologists classify the disease by the affected areas. Ileocolic Crohn's disease, which affects both the ileum (the last part of the small intestine that connects to the large intestine) and the large intestine, accounts for fifty percent of cases. Crohn's ileitis, affecting the ileum only, accounts for thirty percent of cases, and Crohn's colitis, affecting the large intestine, accounts for the remaining twenty percent of cases, and may be particularly difficult to distinguish from ulcerative colitis. The disease can attack any part of the digestive tract, from mouth to anus. However, individuals affected by the disease rarely fall outside these three classifications, being affected in other parts of the gastrointestinal tract such as the stomach and esophagus.
Crohn's disease may also be classified by the behaviour of disease as it progresses. This was formalized in the Vienna classification of Crohn's disease. There are three categories of disease presentation in Crohn's disease: stricturing, penetrating, and inflammatory. Stricturing disease causes narrowing of the bowel which may lead to bowel obstruction or changes in the caliber of the feces. Penetrating disease creates abnormal passageways ( fistulae) between the bowel and other structures such as the skin. Inflammatory disease (or non-stricturing, non-penetrating disease) causes inflammation without causing strictures or fistulae.
Symptoms
Many people with Crohn's disease have symptoms for years prior to the diagnosis. The usual onset is between 15 and 30 years of age, with no difference between men and women. Because of the patchy nature of the gastrointestinal disease and the depth of tissue involvement, initial symptoms can be more vague than with ulcerative colitis.
- Gastrointestinal symptoms
Abdominal pain may be the initial symptom of Crohn's disease. The pain is commonly crampy and may be relieved by defecation. It is often accompanied by diarrhea, which may be bloody. The nature of the diarrhea in Crohn's disease depends on the part of the small intestine or colon that is involved. Ileitis typically results in large-volume watery feces. Colitis may result in a smaller volume of feces of higher frequency. Fecal consistency may range from solid to watery. In severe cases, an individual may have more than 20 bowel movements per day and may need to awaken at night to defecate. Visible bleeding in the feces is less common in Crohn's disease than in ulcerative colitis, but may be seen in the setting of Crohn's colitis. Bloody bowel movements are typically intermittent, and may be bright or dark red in colour. In the setting of severe Crohn's colitis, bleeding may be copious. Flatus and bloating may also add to the intestinal discomfort.
Symptoms caused by intestinal stenosis are also common in Crohn's disease. Abdominal pain is often most severe in areas of the bowel with stenoses. In the setting of severe stenosis, vomiting and nausea may indicate the beginnings of small bowel obstruction. Crohn's disease may also be associated with primary sclerosing cholangitis, a type of inflammation of the bile ducts.
Peri-anal discomfort may also be prominent in Crohn's disease. Itchiness or pain around the anus may be suggestive of inflammation, fistulization or abscess around the anal area or anal fissure. Perianal skin tags are also common in Crohn's disease. Fecal incontinence may accompany peri-anal Crohn's disease. At the opposite end of the gastrointestinal tract, the mouth may be affected by non-healing sores ( aphthous ulcers). Rarely, the esophagus, and stomach may be involved in Crohn's disease. These can cause symptoms including difficulty swallowing ( odynophagia), upper abdominal pain, and vomiting.
- Systemic symptoms
Crohn's disease, like many other chronic, inflammatory diseases, can cause a variety of systemic symptoms. Among children, growth failure is common. Many children are first diagnosed with Crohn's disease based on inability to maintain growth. As Crohn's disease may manifest at the time of the growth spurt in puberty, up to 30% of children with Crohn's disease may have retardation of growth. Fever may also be present, though fevers greater than 38.5 ˚C are uncommon unless there is a complication such as an abscess Among older individuals, Crohn's disease may manifest as weight loss. This is usually related to decreased food intake, since individuals with intestinal symptoms from Crohn's disease often feel better when they do not eat. People with extensive small intestine disease may also have malabsorption of carbohydrates or lipids, which can further exacerbate weight loss.
- Extraintestinal symptoms
In addition to systemic and gastrointestinal involvement, Crohn's disease can affect many other organ systems. Inflammation of the interior portion of the eye, known as uveitis, can cause eye pain, especially when exposed to light ( photophobia). Inflammation may also involve the white part of the eye ( sclera), a condition called episcleritis. Both episcleritis and uveitis can lead to loss of vision if untreated.
Crohn's disease is associated with a type of rheumatologic disease known as seronegative spondyloarthropathy. This group of diseases is characterized by inflammation of one or more joints ( arthritis) or muscle insertions ( enthesitis). The arthritis can affect larger joints such as the knee or shoulder or may exclusively involve the small joints of the hand and feet. The arthritis may also involve the spine, leading to ankylosing spondylitis if the entire spine is involved or simply sacroiliitis if only the lower spine is involved. The symptoms of arthritis include painful, warm, swollen, stiff joints and loss of joint mobility or function.
Crohn's disease may also involve the skin, blood, and endocrine system. One type of skin manifestation, erythema nodosum, presents as red nodules usually appearing on the shins. Erythema nodosum is due to inflammation of the underlying subcutaneous tissue and is characterized by septal panniculitis. Another skin lesion, pyoderma gangrenosum, is typically a painful ulcerating nodule. Crohn's disease also increases the risk of blood clots; painful swelling of the lower legs can be a sign of deep venous thrombosis, while difficulty breathing may be a result of pulmonary embolism. Autoimmune hemolytic anaemia, a condition in which the immune system attacks the red blood cells, is also more common in Crohn's disease and may cause fatigue, pallor, and other symptoms common in anaemia. Clubbing, a deformity of the ends of the fingers, may also be a result of Crohn's disease. Finally, Crohn's disease may cause osteoporosis, or thinning of the bones. Individuals with osteoporosis are at increased risk of bone fractures.
- Complications
Crohn's disease can lead to several mechanical complications within the intestines, including obstruction, fistulae, and abscesses. Obstruction typically occurs from strictures or adhesions which narrow the lumen, blocking the passage of the intestinal contents. Fistulae can develop between two loops of bowel, between the bowel and bladder, between the bowel and vagina, and between the bowel and skin. Abscesses are walled off collections of infection and can occur in the abdomen or in the perianal area in Crohn's disease sufferers.
Crohn's disease also increases the risk of cancer in the area of inflammation. For example, individuals with Crohn's disease involving the small bowel are at higher risk for small intestinal cancer. Similarly, people with Crohn's colitis are at a higher risk for colon cancer. Screening for colon cancer with colonoscopy is recommended for anyone who has had Crohn's colitis for eight years, or more.
Individuals with Crohn's disease are at risk of malnutrition for many reasons, including decreased food intake and malabsorption. The risk increases following resection of the small bowel. Such individuals may require oral supplements to increase their caloric intake, or in severe cases, total parenteral nutrition (TPN). Most people with severe Crohn's disease are referred to a dietitian for assistance in nutrition.
Cause
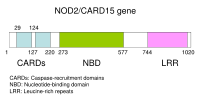
The exact cause of Crohn's disease is unknown. However, genetic and environmental factors have been invoked in the pathogenesis of the disease. Mutations in the CARD15 gene (also known as the NOD2 gene) are associated with Crohn's disease and with susceptibility to certain phenotypes of disease location and activity.
Many environmental factors have also been hypothesized as causes or risk factors for Crohn's disease. Diets high in sweet, fatty or refined foods may play a role. A retrospective Japanese study found that those diagnosed with Crohn's disease had higher intakes of sugar, fat, fish and shellfish than controls prior to diagnosis. A similar study in Israel also found higher intakes of fats (especially chemically modified fats) and sucrose, with lower intakes of fructose and fruits, water, potassium, magnesium and vitamin C in the diets of Crohn's disease sufferers before diagnosis, and cites three large European studies in which sugar intake was significantly increased in people with Crohn's disease compared with controls.
Smoking has been shown to increase the risk of the return of active disease, or "flares". Oral contraceptives have also shown an association with the development of Crohn's disease.
Abnormalities in the immune system have often been invoked as causes of Crohn's disease. It has been hypothesized that Crohn's disease involves augmentation of the Th1 of cytokine response in inflammation. Also, as the colon is rich in bacteria, many infectious agents have been suggested as causes of Crohn's disease, including Mycobacterium avium subspecies paratuberculosis.
Pathophysiology
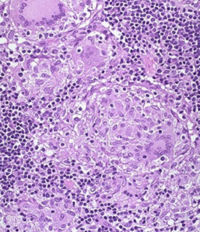
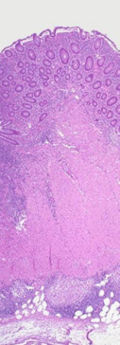
At the time of colonoscopy, biopsies of the colon are often taken in order to confirm the diagnosis. There are certain characteristic features of the pathology seen that point toward Crohn's disease. Crohn's disease shows a transmural pattern of inflammation, meaning that the inflammation may span the entire depth of the intestinal wall. Grossly, ulceration is an outcome seen in highly active disease. There is usually an abrupt transition between unaffected tissue and the ulcer. Under a microscope, biopsies of the affected colon may show mucosal inflammation. Transmural inflammation results in formation of lymphoid aggregates throughout the wall of the colon. This inflammation is characterized by focal infiltration of neutrophils, a type of inflammatory cell, into the epithelium. This typically occurs in the area overlying lymphoid aggregates. These neutrophils, along with mononuclear cells, may infiltrate into the crypts leading to inflammation (crypititis) or abscess (crypt abscess). Granulomas, aggregates of macrophage derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. The granulomas of Crohn's disease do not show "caseation", a cheese-like appearance on microscopic examination that is characteristic of granulomas associated with infections such as tuberculosis. Biopsies may also show chronic mucosal damage as evidenced by blunting of the intestinal villi, atypical branching of the crypts, and change in the tissue type ( metaplasia). One example of such metaplasia, Paneth cell metaplasia, involves development of Paneth cells (typically found in the small intestine) in other parts of the gastrointestinal system.
Diagnosis
The diagnosis of Crohn's disease can sometimes be challenging, and a number of tests are often required to assist the physician in making the diagnosis.
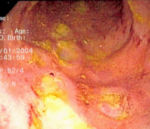
- Endoscopy
A colonoscopy is the best test for making the diagnosis of Crohn's disease as it allows direct visualization of the colon and the terminal ileum, identifying the pattern of disease involvement. During the procedure, the gastroenterologist can also perform a biopsy, taking small samples of tissue for laboratory analysis which may help confirm a diagnosis. As 30% of Crohn's disease involves only the ileum, cannulation of the terminal ileum is required in making the diagnosis. Finding a patchy distribution of disease, with involvement of the colon or ileum but not the rectum, is suggestive of Crohn's disease, as are other endoscopic stigmata.
Wireless capsule endoscopy is a technique where a small capsule with a built-in camera is swallowed, the camera takes serial pictures of the entire gastrointestinal tract and is passed in the patient's faeces. It has been used in the search for Crohn's disease in the small bowel, which cannot be reached with colonoscopy or gastroscopy.The utility of capsule endoscopy for this, however, is still uncertain.
- Radiologic tests
A small bowel follow-through may suggest the diagnosis of Crohn's disease and is useful when the disease involves only the small intestine. Because colonoscopy and gastroscopy allow direct visualization of only the terminal ileum and beginning of the duodenum, they cannot be used to evaluate the remainder of the small intestine. As a result, a barium follow-through x-ray, wherein barium sulfate suspension is ingested and fluoroscopic images of the bowel are taken over time, is useful for looking for inflammation and narrowing of the small bowel. Barium enemas, in which barium is inserted into the rectum and fluoroscopy used to image the bowel, are rarely used in the work-up of Crohn's disease due to the advent of colonoscopy. They remain useful for identifying anatomical abnormalities when strictures of the colon are too small for a colonoscope to pass through, or in the detection of colonic fistulae.
CT and MRI scans are useful for evaluating the small bowel with enteroclysis protocols.They are additionally useful for looking for intra-abdominal complications of Crohn's disease such as abscesses, small bowel obstruction, or fistulae. Magnetic resonance imaging (MRI) are another option for imaging the small bowel as well as looking for complications, though it is more expensive and less readily available
- Blood tests
A complete blood count may reveal anaemia, which may be caused either by blood loss or vitamin B12 deficiency. The latter may be seen with ileitis because vitamin B12 is absorbed in the ileum. Erythrocyte sedimentation rate, or ESR, and C-reactive protein measurements can also be useful to gauge the degree of inflammation. Testing for anti- Saccharomyces cerevisiae antibodies (ASCA) and anti-neutrophil cytoplasmic antibodies (ANCA) has been evaluated to identify inflammatory diseases of the intestine and to differentiate Crohn's disease from ulcerative colitis.
Comparison with ulcerative colitis
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Terminal ileum involvement | Commonly | Never |
| Colon involvement | Usually | Always |
| Rectum involvement | Seldom | Usually |
| Involvement around the anus | Common | Seldom |
| Bile duct involvement | Lower rate of primary sclerosing cholangitis | Higher rate |
| Distribution of Disease | Patchy areas of inflammation | Continuous area of inflammation |
| Endoscopy | Deep geographic and serpiginous (snake-like) ulcers | Continuous ulcer |
| Depth of inflammation | May be transmural, deep into tissues | Shallow, mucosal |
| Fistulae | Common | Seldom |
| Stenosis | Common | Seldom |
| Autoimmune disease | Widely regarded as an autoimmune disease | No consensus |
| Cytokine response | Associated with Th1 | Vaguely associated with Th2 |
| Granulomas on biopsy | Can have granulomas | Granulomas uncommon |
| Surgical cure | Often returns following removal of affected part | Usually cured by removal of colon |
| Smoking | Higher risk for smokers | Lower risk for smokers |
Treatment
Treatment is only needed for people exhibiting symptoms. The therapeutic approach to Crohn's disease is sequential: to treat acute disease, and then to maintain remission. Treatment initially involves the use of medications to treat any infection and to reduce inflammation. This usually involves the use of aminosalicylate anti-inflammatory drugs and corticosteroids, and may include antibiotics. Surgery may be required for complications such as obstructions or abscesses, or if the disease does not respond to drugs within a reasonable time.
Once remission is induced, the goal of treatment becomes maintenance of remission, avoiding flares. Because of side-effects, the prolonged use of corticosteroids must be avoided. Although some people are able to maintain remission with aminosalicylates alone, many require immunosuppressive drugs.
- Drugs
Various drug approaches may be used in Crohn's disease to both obtain and maintain remission. Aminosalicylate anti-inflammatory drugs commonly prescribed are mesalazine (mesalamine, 5-ASA) and the derivative sulfasalazine. The corticosteroids prednisone and budesonide are immunosuppressants, as well as azathioprine (Imuran), 6-mercaptopurine (6-MP), infliximab (Remicade®), methotrexate. Rarely, atypical medications such as thalidomide can be used. The antibiotics metronidazole and ciprofloxacin may also be used for people with colonic disease.
- Surgery
Surgery is generally reserved for complications of Crohn's disease, or when disease that resists treatment with drugs is confined to one location that can be removed. Surgery is often used to manage complications of Crohn's disease, including fistulae, small bowel obstruction, colon cancer, small intestine cancer and fibrostenotic strictures, when strictureplasty (expansion of the stricture) is sometimes performed. Otherwise, and for other complications, resection and anastomosis - the removal of the affected section of intestine and the rejoining of the healthy sections - is the surgery usually performed for Crohn's disease (e.g., ileocolonic resection). Neither type of surgery cures Crohn's disease, as recurrence often reappears in previously unaffected areas of the intestine.
Small intestine transplants are experimental, and are usually only performed when there is a risk of short bowel syndrome due to repeated resection surgeries.
- Diet and lifestyle
There is no evidence that diet causes or cures Crohn's disease, but many people with Crohn's disease note that certain foods improve or worsen their symptoms. Fish oil has been found to be effective in reducing the chance of relapse in less severe cases. People with lactose intolerance due to small bowel disease may benefit from avoiding lactose-containing foods. Many diets have been proposed for treatment of Crohn's disease, and many do improve symptoms, but none have been proven to actually cure Crohn's disease. A low residue diet may be used to reduce the volume of stools excreted daily. Stress can make symptoms of Crohn's disease worse. People with Crohn's disease can find that their symptoms improve with effective stress management.
Because the terminal ileum is the most common site of involvement and is the site for vitamin B12 absorption, people with Crohn's disease are at risk for B12 deficiency and may need supplementation. In cases with extensive small intestine involvement, the fat soluble vitamins A, D, E and K can be deficient. Folate deficiency is a risk when being treated with methotrexate.
- Complementary and alternative medicine
More than half of Crohn's disease sufferers have tried complementary or alternative therapy. These include diets, probiotics, fish oil and other herbal and nutritional supplements. The benefit of these medications is uncertain.
Prognosis
Crohn's disease is a chronic condition that cannot be cured. It is characterized by periods of improvement followed by episodes when symptoms flare up. With treatment, most people achieve a healthy height and weight, and the mortality rate for the disease is low. Crohn's disease is associated with an increased risk of small bowel and colorectal carcinoma.
Epidemiology
The incidence of Crohn's disease has been ascertained from population studies in Norway and the United States and is similar at 6 to 7.1:100,000. Crohn's disease is more common in northern countries, and shows a higher preponderance in northern areas of the same country. The incidence of Crohn's disease in North America is 6:100,000, and is thought to be similar in Europe, but lower in Asia and Africa. It also has a higher incidence in Ashkenazi Jews.
Crohn's disease has a bimodal distribution in incidence as a function of age: the disease tends to strike people in their teens and twenties, and people in their fifties through seventies. It is rare in early childhood. There is no association with gender, social class or occupation. Parents, siblings or children of people with Crohn's disease are 3 to 20 times more likely to develop the disease. Twin studies show a concordance of greater than 55% for Crohn's disease.
History
Inflammatory bowel diseases were described by Giovanni Battista Morgagni (1682-1771), by Polish surgeon Antoni Leśniowski in 1904 (leading to the use of the eponym "Leśniowski-Crohn disease" in Poland) and by Scottish physician T. Kennedy Dalziel in 1913.
Burrill Bernard Crohn, an American gastroenterologist at Mount Sinai Hospital, described fourteen cases in 1932, and submitted them to the American Medical Association under the rubrick of "Terminal ileitis: A new clinical entity". Later that year, he, along with colleagues Leon Ginzburg and Gordon Oppenheimer published the case series as "Regional ileitis: a pathologic and clinical entity".