ABO blood group system
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
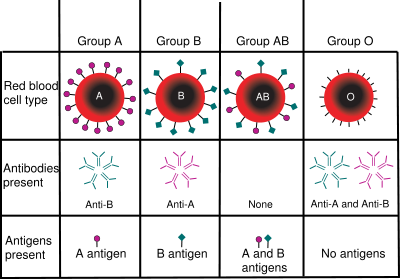
The ABO blood group system is the most important blood type system (or blood group system) in human blood transfusion. The associated anti-A antibodies and anti-B antibodies are usually IgM antibodies, which are usually produced in the first years of life by sensitization to environmental substances such as food, bacteria and viruses. ABO blood types are also present in some animals, for example apes such as chimpanzees, bonobos and gorillas.
ABO antigens
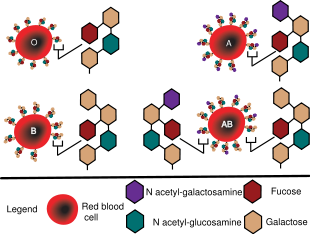
The A antigen and the B antigen are derived from a common precursor known as the H antigen (or H substance). The H antigen is a glycosphingolipid ( sphingolipid with carbohydrates linked to the ceramide moiety). Since it lacks N-acetylneuraminic acid ( sialic acid) it is referred to as a globoside, not a ganglioside. In blood group O the H antigen remains unchanged and consists of a chain of galactose, N-Acetylglucosamine, galactose, and fucose attached to the ceramide. H antigens can be changed into A or B antigens by enzymes coded by the blood group A or B genes. Type A has an extra N-Acetylgalactosamine bonded to the galactose near the end, while type B has an extra galactose bonded to the galactose near the end.
Individuals with Type A blood can accept blood from donors of type A and type O blood. Individuals with type B blood can receive blood from donors of type B and type O blood. Individuals with type AB blood may receive blood from donors of type A, type B, type AB, or type O blood. Type AB blood is referred to as the universal recipient. Individuals of type O blood may receive blood from donors of type O blood. Type O blood is called the universal donor.
Antibodies are not formed against the H antigen, except by those with the Bombay phenotype.
In ABH secretors, ABH antigens are secreted by most mucous-producing cells of the body interfacing with the environment, including lung, skin, liver, pancreas, stomach, intestines, ovaries and prostate.
History of discoveries
The ABO blood group system is widely credited to have been discovered by the Austrian scientist Karl Landsteiner, who found three different blood types in 1900; he was awarded the Nobel Prize in Physiology or Medicine in 1930 for his work. Due to inadequate communication at the time it was subsequently found that Czech serologist Jan Janský had independently pioneered the classification of human blood into four groups, but Landsteiner's independent discovery had been accepted by the scientific world while Janský remained in relative obscurity. Janský's classification is however still used in Russia and states of former USSR (see below). In America Moss published his own (very similar) work in 1910.
Landsteiner described A, B, and O; Decastrello and Sturli discovered the fourth type, AB, in 1902. Ludwik Hirszfeld and E. von Dungern discovered the heritability of ABO blood groups in 1910-11, with Felix Bernstein demonstrating the correct blood group inheritance pattern of multiple alleles at one locus in 1924.
Serology
Anti-A and anti-B antibodies, which are not present in the newborn, appear in the first years of life. It is possible that food and environmental antigens (bacterial, viral or plant antigens) are similar enough to A and B glycoprotein antigens that antibodies created against the environmental antigens in the first years of life can cross react with ABO-incompatible red blood cells. Anti-A and anti-B antibodies are usually IgM, which are not able to pass through the placenta to the fetal blood circulation.
The "Light in the Dark theory" however suggests that when budding viruses take with them host cell membranes (in particular from the lung and mucosal epithelium where they are highly expressed)they also take along ABO Blood antigens from those membranes, and may carry them into secondary recipients where these antigens can elicit a host immune response againts these non-self foreign blood antigens. These viral carried blood antigens may be responsible for priming newborns into producing neutralizing antibodies against foreign blood antigens. Support for this theory has come to light in recent experiments with HIV. HIV can be neutralized in "in-vitro" experiments using antibodies against blood group antigens specifically expressed on the HIV producing cell lines. The "Light in the Dark theory" suggests a new novel evolutionary hypothesis that there is true communal immunity, which has developed to reduce the inter-transmissibility of viruses within a population. It suggests that individuals in a population supply and make a diversity of unique antigenic moieties so as to keep the population as a whole more resistant to infection. A system set up ideally to work with variable recessive alleles.
ABO hemolytic disease of the newborn
ABO blood group incompatibilities between the mother and child does not usually cause hemolytic disease of the newborn (HDN) because antibodies to the ABO blood groups are usually of the IgM type, which do not cross the placenta; however, sometimes IgG ABO antibodies are produced and a baby can develop ABO hemolytic disease of the newborn.
Inheritance
| Blood group inheritance | ||||
| Mother/Father | O | A | B | AB |
|---|---|---|---|---|
| O | O | O, A | O, B | A, B |
| A | O, A | O, A | O, A, B, AB | A, B, AB |
| B | O, B | O, A, B, AB | O, B | A, B, AB |
| AB | A, B | A, B, AB | A, B, AB | A, B, AB |
Blood groups are inherited from both parents. The ABO blood type is controlled by a single gene with three alleles: i, IA, and IB. The gene encodes a glycosyltransferase - that is, an enzyme that modifies the carbohydrate content of the red blood cell antigens. The gene is located on the long arm of the ninth chromosome (9q34).
IA allele gives type A, IB gives type B, and i gives type O. IA and IB are dominant over i, so ii people have type O, IAIA or IAi have A, and IBIB or IBi have type B. IAIB people have both phenotypes because A and B express a special dominance relationship: codominance, which means that type A and B parents can have an AB child. Thus, it is extremely unlikely for a type AB parent to have a type O child (it is not, however, direct proof of illegitimacy): the cis-AB phenotype has a single enzyme that creates both A and B antigens. The resulting red blood cells do not usually express A or B antigen at the same level that would be expected on common group A1 or B red blood cells, which can help solve the problem of an apparently genetically impossible blood group.
Evolutionary biologists theorize that the IA allele evolved earliest, followed by O (by the deletion of a single nucleotide, shifting the reading frame) and then IB. This chronology accounts for the percentage of people worldwide with each blood type. It is consistent with the accepted patterns of early population movements and varying prevalent blood types in different parts of the world: for instance, B is very common in populations of Asian descent, but rare in ones of Western European descent.)
Population data
| Distribution of blood types among various populations | ||||
| Population | O | A | B | AB |
|---|---|---|---|---|
| Native South Americans | 100% | – | – | – |
| British | 46% | 42% | 9% | 3% |
| Irish | 52% | 35% | 10% | 3% |
| French | 43% | 45% | 9% | 3% |
| Hongkonger | 40% | 26% | 27% | 7% |
| Vietnamese | 45.0% | 21.4% | 29.1% | 4.5% |
| Australian aboriginals | 44.4% | 55.6% | – | – |
| Germans | 42.8% | 41.9% | 11.0% | 4.2% |
| Bengalis | 22.0% | 24.0% | 38.2% | 15.7% |
| Saami | 18.2% | 54.6% | 4.8% | 12.4% |
| Finns | 31% | 44% | 17% | 8% |
| Romanians | 34% | 41% | 19% | 6% |
| Russians | 33% | 36% | 23% | 8% |
| Japanese | 30% | 40% | 20% | 10% |
| African Americans | 49% | 27% | 20% | 4% |
| Kenyan | 60% | 19% | 20% | 1% |
The distribution of the blood groups A, B, O and AB varies across the world according to the population or race. There are also variations in blood type distribution within human subpopulations.
In the UK the distribution of blood type frequencies through the population still shows some correlation to the distribution of placenames and to the successive invasions and migrations including Vikings, Danes, Saxons, Celts, and Normans who contributed the morphemes to the placenames and the genes to the population.
Association with von Wilebrand factor
The ABO antigen is also expressed on the von Willebrand factor (vWF) glycoprotein, which participates in hemostasis (control of bleeding). In fact, having type O blood predisposes to bleeding, as 30% of the total genetic variation observed in plasma vWF is explained by the effect of the ABO blood group, and individuals with group O blood normally have significantly lower plasma levels of vWF (and Factor VIII) than do non-O individuals. In addition, vWF is degraded more rapidly due to the higher prevalence of blood group O with the Cys1584 variant of vWF (an amino acid polymorphism in VWF): the gene for ADAMTS13 (vWF-cleaving protease) maps to the ninth chromosome (9q34), the same locus as ABO blood type. Higher levels of vWF are more common amongst people who have had ischaemic stroke (from blood clotting) for the first time. The results of this study found that the occurrence was not affected by ADAMTS13 polymorphism, and the only significant genetic factor was the person's blood group.
Bombay phenotype
Individuals with the rare Bombay phenotype ( hh) do not express substance H on their red blood cells, and therefore do not bind A or B antigens. Instead, they produce antibodies to substance H (which is present on all red cells except those of hh genotype) as well as to both A and B antigens, and are therefore compatible only with other hh donors.
Nomenclature in Europe former USSR
In parts of Europe the "O" in ABO blood type is substituted with "0" (zero), signifying the lack of A or B antigen. In the former USSR and Russia, blood types are referenced using numbers and Roman numerals instead of letters. This is Janský's original classification of blood types. It designates the blood types of humans as I, II, III, and IV, which are elsewhere designated, respectively, as O, A, B, and AB. The designation A and B with reference to blood groups was proposed by Hirszfeld.
Examples of ABO and Rhesus D slide testing method
In the slide testing method shown above, three drops of blood are placed on a glass slide with liquid reagents. Agglutination indicates the presence of blood group antigens in the blood.
Universal blood created from other types
In April 2007 an international team of researchers announced in the journal Nature Biotechnology an inexpensive and efficient way to convert types A, B and AB blood into type O. This is done by using glycosidase enzymes from specific bacteria to strip the blood group antigens from red blood cells. The removal of A and B antigens still does not address the problem of the Rhesus blood group antigen on the blood cells of Rhesus positive individuals, and so blood from Rhesus negative donors must be used. Patient trials will be conducted before the method can be relied on in live situations.