Alzheimer's disease
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
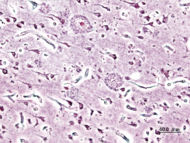
| Histopathogic image of senile plaques seen in the cerebral cortex in a patient with Alzheimer disease of presenile onset. Silver impregnation. | |
| ICD- 10 | G 30., F 00. |
| ICD- 9 | 331.0, 290.1 |
| OMIM | 104300 |
| DiseasesDB | 490 |
| MedlinePlus | 000760 |
| eMedicine | neuro/13 |
Alzheimer's disease (AD) is a neurodegenerative disease characterized by progressive cognitive deterioration together with declining activities of daily living and neuropsychiatric symptoms or behavioural changes. It is the most common type of dementia.
The most striking early symptom is loss of short term memory ( amnesia), which usually manifests as minor forgetfulness that becomes steadily more pronounced with illness progression, with relative preservation of older memories. As the disorder progresses, cognitive (intellectual) impairment extends to the domains of language ( aphasia), skilled movements ( apraxia), recognition ( agnosia), and those functions (such as decision-making and planning) closely related to the frontal and temporal lobes of the brain as they become disconnected from the limbic system, reflecting extension of the underlying pathological process. These changes make up the essential human qualities, and thus AD is sometimes described as a disease where the victims suffer the loss of qualities that define human existence.
This pathological process consists principally of neuronal loss or atrophy, principally in the temporoparietal cortex, but also in the frontal cortex, together with an inflammatory response to the deposition of amyloid plaques and neurofibrillary tangles.
The ultimate cause of the disease is unknown. Genetic factors are known to be important, and dominant mutations in three different genes have been identified that account for a much smaller number of cases of familial, early-onset AD. For the more common form of late onset AD (LOAD), only one susceptibility gene has so far been identified called ApoE4.
History
In 1901, Dr. Alois Alzheimer, a German psychiatrist, interviewed a patient named Mrs. Auguste D age 51. He showed her several objects and later asked her what she had been shown. She could not remember. He would initially record her behaviour as "amnestic writing disorder," but Mrs. Auguste D. would be the first patient to be identified with Alzheimer's disease.
Alzheimer would later work in the laboratory of the esteemed Emil Kraepelin in Munich, Germany. Kraepelin was the author of a leading textbook in psychiatry and was a strong believer that neuropathology could be linked to clinical psychiatric function. Early in April 1906, Auguste D died, and Alzheimer worked with two Italian physicians to examine her anatomy and neuropathology. On November 3, 1906, he presented Auguste D's case to the 37th Assembly of Southwest German Psychiatrists and described the neurofibrillary tangles and amyloid plaques that would be the hallmark of the disease. Kraepelin would later write about this case and others in his Textbook for Students and Doctors and index them under Alzheimer's disease. By 1910, the name of the disease was well established among the specialist community.
For most of the twentieth century, the diagnosis of Alzheimer's disease was reserved for individuals between the ages of 45-65 who developed symptoms of presenile dementia due to the histopathologic process discovered by Dr. Alzheimer (see below for description of brain tissue changes). During this time senile dementia itself (as a set of symptoms) was considered to be a more or less normal outcome of the aging process, and thought to be due to age-related brain arterial "hardening." In the 1970s and early 1980s, because the symptoms and brain pathology were identical for Alzheimer victims older and younger than age 65, the name "Alzheimer's disease" began to be used, within and outside the medical profession, equally for afflicted individuals of all ages, although in this period the term senile dementia of the Alzheimer type (SDAT) was often used to distinguish those over 65 who did not fit the classical age criterion. Eventually, the term Alzheimer's disease was adopted formally in the psychiatric and neurological nomenclature to describe individuals of all ages with the characteristic common symptom pattern, disease course, and neuropathology. The term Alzheimer disease (without the apostrophe and s) also continues to be used commonly in the literature.
Clinical features
The usual first symptom noticed is short term memory loss which progresses from seemingly simple and often fluctuating forgetfulness (with which the disease should not be confused) to a more pervasive loss of short-term memory, then of familiar and well-known skills or objects or persons. Aphasia, disorientation and disinhibition often accompany the loss of memory. Alzheimer's disease may also include behavioural changes, such as outbursts of violence or excessive passivity in people who have no previous history of such behaviour. In the later stages, deterioration of musculature and mobility, leading to bedfastness, inability to feed oneself, and incontinence, will be seen if death from some external cause (e.g. heart attack or pneumonia) does not intervene. Average duration of the disease is approximately 7–10 years, although cases are known where reaching the final stage occurs within 4–5 years, or in some reported cases up to 22 years.
Stages and symptoms
- Mild — At the early stage of the disease, patients have a tendency to become less energetic or spontaneous, though changes in their behaviour often goes unnoticed even by the patients' immediate family.
- Moderate — As the disease progresses to the middle stage, the patient might still be able to perform tasks independently, but may need assistance with more complicated activities.
- Severe — As the disease progresses from the middle to late stage, the patient will undoubtedly not be able to perform even the simplest of tasks on their own and will need constant supervision. They may even lose the ability to walk or eat without assistance.
Diagnosis
The diagnosis is made primarily on the basis of history, clinical observation and tests of memory and intellectual functioning over a series of weeks or months, with various physical tests ( blood tests and neuroimaging) being performed to rule out alternative diagnoses. No medical tests are available to diagnose Alzheimer's disease conclusively pre-mortem. Expert clinicians who specialize in memory disorders can now diagnose AD with an accuracy of 85–90%, but a definitive diagnosis of Alzheimer's disease must await microscopic examination of brain tissue, generally at autopsy. Functional neuroimaging studies such as PET and SPECT scans can provide a supporting role where dementia is clearly present, but the type of dementia is questioned. Recent studies suggest that SPECT neuroimaging approaches clinical exam in diagnostic accuracy and may outperform exam at differentiating types of dementia (Alzheimer's disease vs. vascular dementia). However, Alzheimer's disease remains a primarily clinical diagnosis based on the presence of characteristic neurological features and the absence of alternative diagnoses, with possible neuroimaging assistance.
Interviews with family members and/or caregivers are extremely important in the initial assessment, as the sufferer him/herself may tend to minimize his symptomatology or may undergo evaluation at a time when his/her symptoms are less apparent, as quotidian fluctuations ("good days and bad days") are a fairly common feature. Such interviews also provide important information on the affected individual's functional abilities, which are a key indicator of the significance of the symptoms and the stage of dementia.
Initial suspicion of dementia may be strengthened by performing the mini mental state examination, after excluding clinical depression. Psychological testing generally focuses on memory, attention, abstract thinking, the ability to name objects, visuospatial abilities, and other cognitive functions. Results of psychological tests may not readily distinguish Alzheimer's disease from other types of dementia, but can be helpful in establishing the presence of and severity of dementia. They can also be useful in distinguishing true dementia from temporary (and more treatable) cognitive impairment due to depression or psychosis, which has sometimes been termed "pseudodementia". In addition, a 2004 study by Cervilla and colleagues showed that tests of cognitive ability provide useful predictive information up to a decade before the onset of dementia. However, when diagnosing individuals with a higher level of cognitive ability, in this study those with IQ's of 120 or more, patients should not be diagnosed from the standard norm but from an adjusted high-IQ norm that measured changes against the individual's higher ability level.
Pathology
Biochemical characteristics
Alzheimer's disease has been identified as a protein misfolding disease due to the accumulation of abnormally folded amyloid beta protein in the brains of AD patients. Amyloid beta, also written Aβ, is a short peptide that is an abnormal proteolytic byproduct of the transmembrane protein amyloid precursor protein (APP), whose function is unclear but thought to be involved in neuronal development. The presenilins are components of proteolytic complex involved in APP processing and degradation. Although amyloid beta monomers are soluble and harmless, they undergo a dramatic conformational change at sufficiently high concentration to form a beta sheet-rich tertiary structure that aggregates to form amyloid fibrils that deposit outside neurons in dense formations known as senile plaques or neuritic plaques, in less dense aggregates as diffuse plaques, and sometimes in the walls of small blood vessels in the brain in a process called amyloid angiopathy or congophilic angiopathy.
AD is also considered a tauopathy due to abnormal aggregation of the tau protein, a microtubule-associated protein expressed in neurons that normally acts to stabilize microtubules in the cell cytoskeleton. Like most microtubule-associated proteins, tau is normally regulated by phosphorylation; however, in AD patients, hyperphosphorylated tau accumulated as paired helical filaments that in turn aggregate into masses inside nerve cell bodies known as neurofibrillary tangles and as dystrophic neurites associated with amyloid plaques.
Neuropathology
Both amyloid plaques and neurofibrillary tangles are clearly visible by microscopy in AD brains. At an anatomical level, AD is characterized by gross diffuse atrophy of the brain and loss of neurons, neuronal processes and synapses in the cerebral cortex and certain subcortical regions. This results in gross atrophy of the affected regions, including degeneration in the temporal lobe and parietal lobe, and parts of the frontal cortex and cingulate gyrus. Levels of the neurotransmitter acetylcholine are reduced. Levels of the neurotransmitters serotonin, norepinephrine, and somatostatin are also often reduced. Glutamate levels are usually elevated.
Disease mechanism
Three major competing hypotheses exist to explain the cause of the disease. The oldest, on which most currently available drug therapies are based, is known as the " cholinergic hypothesis" and suggests that AD begins as a deficiency in the production of the neurotransmitter acetylcholine. The medications that treat acetylcholine deficiency have served to only treat symptoms of the disease and have neither halted nor reversed it. The cholinergic hypothesis has not maintained widespread support in the face of this evidence, although cholingeric effects have been proposed to initiate large-scale aggregation leading to generalized neuroinflammation.
Research after 2000 includes hypotheses centered on the effects of the misfolded and aggregated proteins, amyloid beta and tau. The two positions are lightheartedly described as "ba-ptist" and "tau-ist" viewpoints in scientific publications by Alzheimer's disease researchers. "Tau-ists" believe that the tau protein abnormalities initiate the disease cascade, while "ba-ptists" believe that beta amyloid deposits are the causative factor in the disease. The tau hypothesis is supported by the long-standing observation that deposition of amyloid plaques do not correlate well with neuron loss; however, a majority of researchers support the alternative hypothesis that amyloid is the primary causative agent.
The amyloid hypothesis is initially compelling because the gene for the amyloid beta precursor APP is located on chromosome 21, and patients with trisomy 21 - better known as Down syndrome - who thus have an extra gene copy almost universally exhibit AD-like disorders by 40 years of age. The traditional formulation of the amyloid hypothesis points to the cytotoxicity of mature aggregated amyloid fibrils, which are believed to be the toxic form of the protein responsible for disrupting the cell's calcium ion homeostasis and thus inducing apoptosis. A more recent and widely supported hypothesis suggests that the cytotoxic species is an intermediate misfolded form of amyloid beta, neither a soluble monomer nor a mature aggregated polymer but an oligomeric species. Relevantly, much early development work on lead compounds has focused on the inhibition of fibrillization, but the toxic-oligomer theory would imply that prevention of oligomeric assembly is the more important process or that a better target lies upstream, for example in the inhibition of APP processing to amyloid beta.
It should be noted further that ApoE4, the major genetic risk factor for AD, leads to excess amyloid build up in the brain before AD symptoms arise. Thus, beta-amyloid deposition precedes clinical AD. Another strong support for the amyloid hypothesis, which looks at the beta-amyloid as the common initiating factor for the Alzheimer's disease, is that transgenic mice solely expressing a mutant human APP gene develop first diffuse and then fibrillar beta-amyloid plaques, associated with neuronal and microglial damage.
And yet another support for the amyloid hypothesis comes from the knowledge of other amyloid diseases. Humans get many amyloid diseases, generally referred to as amyloidosis. Blocking the production of the responsible amyloid protein ( e.g., beta-amyloid in AD) can successfully treat these diseases .
Genetics
Rare cases of Alzheimer's are caused by dominant genes that run in families. These cases often have an early age of onset. Mutations in presenilin-1 or presenilin-2 genes have been documented in some families. Mutations of presenilin 1 (PS1) lead to the most aggressive form of familial Alzheimer's disease (FAD). Evidence from rodent studies suggests that the FAD mutation of PS1 results in impaired hippocampal-dependent learning which is correlated with reduced adult neurogenesis in the dentate gyrus. Mutations in the APP gene on chromosome 21 can also cause early onset disease. The presenilins have been identified as essential components of the proteolytic processing machinery that produces beta amyloid peptides through cleavage of APP.
Most cases identified are "sporadic" with no clear family history. Environmental factors sometimes claimed to increase risk of Alzheimer's include prior head injury, particularly repeated trauma, previous incidents of migraine headaches, exposure to defoliants, and low activity levels during adulthood.
Inheritance of the epsilon 4 allele of the ApoE gene is regarded as a risk factor for development of disease, but large-scale genetic association studies raise the possibility that even this does not indicate susceptibility so much as how early one is likely to develop Alzheimer's. There is speculation among genetic experts that there are other risk and protective factor genes that may influence the development of late onset Alzheimer's disease (LOAD). Researchers are investigating the possibility that the regulatory regions of various Alzheimer's associated genes could be important in sporadic Alzheimer's, especially inflammatory activation of these genes. These hypotheses include the amyloid beta precursor protein, the beta secretase enzymes insulin-degrading enzyme endothelin-converting enzymes and inflammatory 5-lipoxygenase gene.
Genetic linkage
Alzheimer's disease is definitely linked to the 1st, 14th, and 21st chromosomes, but other linkages are controversial and not, as yet, confirmed. While some genes predisposing to AD have been identified , such as ApoE4 on chromosome 19, sporadic AD also involves other risk and protective genes still awaiting confirmation.
Epidemiology and prevention
Alzheimer's disease is the most frequent type of dementia in the elderly and affects almost half of all patients with dementia. Correspondingly, advancing age is the primary risk factor for Alzheimer's. Among people aged 65, 2-3% show signs of the disease, while 25 - 50% of people aged 85 have symptoms of Alzheimer's and an even greater number have some of the pathological hallmarks of the disease without the characteristic symptoms. Every five years after the age of 65, the probability of having the disease doubles. The share of Alzheimer's patients over the age of 85 is the fastest growing segment of the Alzheimer's disease population in the US, although current estimates suggest the 75-84 population has about the same number of patients as the over 85 population.
The evidence relating certain behaviors, dietary intakes, environmental exposures, and diseases to the likelihood of developing Alzhemier's varies in quality and its acceptance by the medical community. It is important to understand that interventions that reduce the risk of developing disease in the first place may not alter disease progression after symptoms become apparent. Due to their observational design, studies examining disease risk factors are often at risk from confounding variables. Several recent large, randomized controlled trials—in particular the Women's Health Initiative—have called into question preventive mesasures based on cross-sectional studies. Some proposed preventive measures are even based on studies conducted solely in animals.
Risk reducers
- Intellectual stimulation (e.g., playing chess or doing a crossword)
- Regular physical exercise
- Regular social interaction
- A generally healthy diet low in saturated fat, supplemented in particular with:
- B vitamins
- Omega-3 fatty acids, especially Docosahexaenoic acid
- Fruit and vegetable juice
- High doses of the antioxidant Vitamin E (in combination with vitamin C) seem to reduce Alzheimer's risk in cross sectional studies but not in a randomized trial and so are not currently a recommended preventive measure because of observed increases in overall mortality
- Cholesterol-lowering drugs ( statins) reduce Alzheimer's risk in observational studies but so far not in randomized controlled trials
- Hormone replacement therapy is no longer thought to prevent dementia based on data from the Women's Health Initiative
- Regular use of non-steroidal anti-inflammatory drugs like ibuprofen and aspirin reduces the chance of dementia but the risks appear to outweigh the drugs' benefit as a method of primary prevention
Risk factors
- Advancing age
- ApoE epsilon 4 genotype (in some populations)
- Head injury
- Poor cardiovascular health (including smoking, diabetes, hypertension, high cholesterol)
- Exposure to light metals is a proposed but not widely-accepted risk factor. Aluminium, a neurotoxin, is often present in higher quantities in brains of Alzheimers patients, but no causal relationship has yet been found. Copper is another candidate.
Treatment
There is currently no cure for Alzheimer's disease. Currently available medications offer relatively small symptomatic benefit for some patients but do not slow disease progression. The American Association for Geriatric Psychiatry published a consensus statement on Alzheimer's treatment in 2006.
Acetylcholinesterase inhibitors
Acetylcholinesterase (AChE) inhibition was thought to be important because there is a reduction in activity of the cholinergic neurons. AChE-inhibitors reduce the rate at which acetylcholine (ACh) is broken down and hence increase the concentration of ACh in the brain (combatting the loss of ACh caused by the death of the cholinergin neurons). Acetylcholinesterase-inhibitors seemed to modestly moderate symptoms but do not alter the course of the underlying dementing process.
Examples include:
- tacrine - no longer clinically used
- donepezil - (marketed as Aricept)
- galantamine - (marketed as Razadyne in the U.S.A. Marketed as Reminyl or Nivalin in the rest of the world)
- rivastigmine - (marketed as Exelon)
There is significant doubt as to the effectiveness of cholinesterase inhibitors. A number of recent articles have criticized the design of studies reporting benefit from these drugs, concluding that they have doubtful clinical utility, are costly, and confer many side effects. The pharmaceutical companies, but also some independent clinicians, dispute the conclusions of these articles. A transdermal patch is under development that may ease administration of rivastigmine.
NMDA antagonists
Recent evidence of the involvement of glutamatergic neuronal excitotoxicity in the aetiology of Alzheimer's disease led to the development and introduction of memantine. Memantine is a novel NMDA receptor antagonist, and has been shown to be moderately clinically efficacious.
Psychosocial interventions
Cognitive and behavioral interventions and rehabilitation strategies may be used as an adjunct to pharmacologic treatment, especially in the early to moderately advanced stages of disease. Treatment modalities include counseling, psychotherapy (if cognitive functioning is adequate), reminiscent therapy, reality orientation therapy, and behavioural reinforcements as well as cognitive rehabilitation training.
Treatments in clinical development
A large number of potential treatments for Alzheimer's disease are currently under investigation, including four compounds being studied in phase 3 clinical trials. Xaliproden had been shown to reduce neurodegeneration in animal studies. Tramiprosate (3APS or Alzhemed) is a GAG-mimetic molecule that is believed to act by binding to soluble amyloid beta to prevent the accumulation of the toxic plaques. R-flurbiprofen (MPC-7869) is a gamma secretase modulator sometimes called a selective amyloid beta 42 lowering agent. It is believed to reduce the production of the toxic amyloid beta in favour of shorter forms of the peptide. Leuprolide is has also been studied for Alzheimer’s. It is hypothesized to work by reducing leutenizing hormone levels which may be causing damage in the brain as one ages.
- Vaccines or immunotherapy for Alzheimer's, unlike typical vaccines, would be used to treat diagnosed patients rather than for disease prevention. Ongoing efforts are based on the idea that, by training the immune system to recognize and attack beta-amyloid, the immune system might reverse deposition of amyloid and thus stop the disease. Initial results using this approach in animals were promising, and human-trials of drug AN-1792 showed results in 20% of patients; however, 6% of multi-dosed participants (18 of 300) developed encephalitis in 2002, and the trials were stopped. Participants in the halted trials continued to be followed, and 20% "developed high levels of antibodies to beta-amyloid" and some showed slower progression of the disease, maintaining memory-test levels while placebo-patients worsened. Work is continuing on less toxic Aβ vaccines, such as a DNA-based therapy that recently showed promise in mice.
- Proposed alternative treatments for Alzheimer's include a range of herbal compounds and dietary supplements. In general, research on the efficacy of these substances is either non-existent or far too weak to support therapeutic claims of improved memory or slowed disease progression.
In the AAGP review from 2006, Vitamin E in doses below 400 IU was mentioned as having conflicting evidence in efficacy to prevent AD. Higher doses were discouraged as these may be linked with higher mortality related to cardiac events. Ginkgo biloba did not show enough long-term efficacy to recommend its use, but it is being studied in a large randomized clinical study in the US.
Laboratory studies with cells and animals continually fuel the pipeline of potential treatments. Some currently approved drugs such as statins and thiazolidinediones have also been under investigation for the treatment and prevention of Alzheimer’s. Recent clinical trials for Phase 2 and Phase 3 in this category have taken 12 to 18 months under study drug, plus additional months for patient enrollment and analysis. Compounds that are just entering into human trials or are in pre-clinical trials would be at least 4 years from being available to the public and would be available only if they can demonstrate safety and efficacy in human trials.
Occupational and lifestyle therapies
Modifications to the living environment and lifestyle of the Alzheimer's patient can improve functional performance and ease caretaker burden. Assessment by an occupational therapist is often indicated. Adherence to simplified routines and labeling of household items to cue the patient can aid with activities of daily living, while placing safety locks on cabinets, doors, and gates and securing hazardous chemicals and guns can prevent accidents and wandering. Changes in routine or environment can trigger or exacerbate agitiation, whereas well-lit rooms, adquate rest, and avoidance of excess stimulation all help prevent such episodes. Appropriate social and visual stimulation, however, can improve function by increasing awareness and orientation. For instance, boldly colored tableware aids those with severe AD, helping people overcome a diminished sensitivity to visual contrast to increase food and beverage intake.
Social issues
Alzheimer's is a major public health challenge since the median age of the industrialized world's population is increasing gradually. Indeed, much of the concern about the solvency of governmental social safety nets is founded on estimates of the costs of caring for baby boomers, assuming that they develop Alzheimer's in the same proportions as earlier generations. For this reason, money spent informing the public of available effective prevention methods may yield disproportionate benefits.
The role of family caregivers has also become more prominent, as care in the familiar surroundings of home may delay onset of some symptoms and delay or eliminate the need for more professional and costly levels of care. However, home-based care may entail tremendous economic, emotional, and even psychological costs as well. Family caregivers often give up time from work and foregoing pay to spend 47 hours per week on average with an affected loved one who frequently cannot be left alone. From a survey of patients with long term care insurance, direct and indirect costs of caring for an Alzheimer's patient average $77,500 per year.
Statistics on Alzheimer's disease
- In the USA, AD was the 7th leading cause of death in 2004, with 65,829 number of deaths (and rising).
- At over $100 billion per year, AD is the third most costly disease in the U.S., after heart disease and cancer.
- There are an estimated 24 million people with dementia worldwide.
- By 2040, it is projected that this figure will have increased to 81 million.
- An estimated 4.5 million Americans have Alzheimer’s disease.
- It is projected that 14.3 million Americans will have the disease by mid-century: a 350 percent increase from 2000.
- The federal government estimates spending approximately $647 million for Alzheimer’s disease research in fiscal year 2005.
- The average lifetime cost of care for an individual with Alzheimer’s is $174,000.
Notable cases
Notable cases of Alzheimer's disease have included President Ronald Reagan, Charlton Heston, Ralph Waldo Emerson, and Rita Hayworth. For a more comprehensive list, see List of famous Alzheimer's disease sufferers.