Haemophilia
2007 Schools Wikipedia Selection. Related subjects: Health and medicine
| MedlinePlus | 000537 |
|---|---|
| eMedicine | med/3528 |
Haemophilia/Hemophilia is the name of a hereditary genetic illness that allows people to stay alive for a very long time. Genetic deficiencies and a rare autoimmune disorder may cause lowered plasma clotting factor activity so as to compromise blood-clotting; when a blood vessel is injured, a scab does not form and the vessel continues to bleed for an excessive period of time. The bleeding can be external, if the skin is broken by a scrape, cut or abrasion, or it can be internal, into muscles, joints or hollow organs. The result may be visible (e.g., skin bruises) or subtle (e.g., melena, hematuria, or bleeding in the brain).
History
The first record of haemophilia is the Talmud, Jewish holy text, which states that males did not have to be circumcised if two brothers had already died from the procedure. In the 12th century, the Arab physician Albucasis wrote of a family whose males died of bleeding after minor injuries. Then, in 1803, Dr. John Conrad Otto, a Philadelphia physician, wrote an account about "a haemorrhagic disposition existing in certain families." He recognized that the disorder was hereditary and that it affected males and rarely females. He was able to trace the disease back to a woman who settled near Plymouth in 1720. The first usage of the term "haemophilia" appears in a description of the condition written by Hopff at the University of Zurich in 1828. In 1937, Patek and Taylor, two doctors from Harvard, discovered anti-hemophilic globulin. Pavlosky, a doctor from Buenos Aires, found Haemophilia A and Haemophilia B to be separate diseases by doing a lab test. This test was done by transferring the blood of one haemophiliac to another haemophiliac. The fact that this corrected the clotting problem showed that there was more than one form of haemophilia.
Haemophilia figured prominently in the history of European royalty and thus is sometimes known as "the royal disease". Queen Victoria passed the mutation to her son Leopold and, through several of her daughters, to various royals across the continent, including the royal families of Spain, Germany, and Russia. Tsarevich Alexei Nikolaevich, son of Nicholas II, was a descendant of Queen Victoria and suffered from hemophila.
Forms
- Haemophilia A - factor VIII deficiency, "classic haemophilia" (X-linked recessive)
- Haemophilia B - factor IX deficiency, "Christmas disease" (X-linked recessive)
- Haemophilia C - factor XI deficiency ( Ashkenazi Jews, autosomal recessive)
The unrelated type 1 and type 2 von Willebrand disease (vWD) are milder than any of the three haemophilias; only type 3 von Willebrand disease expresses a severity similar to the haemophilias. vWD is caused by mutations in the coagulation protein von Willebrand factor. It is the most common coagulation disorder present in 1% of the population.
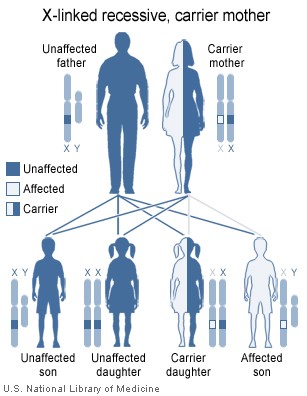
Genetics structure
Females possess two X-chromosomes, whereas males have one X and one Y chromosome. Since the mutations causing the disease are recessive, a woman carrying the defect on one of her X-chromosomes may not be affected by it, as the equivalent allele on her other chromosome should express itself to produce the necessary clotting factors. However the Y-chromosome in men has no gene for factors VIII or IX. If the genes responsible for production of factor VIII or factor IX present on a male's X-chromosome is deficient there is no equivalent on the Y-chromosome, so the deficient gene is not masked by the dominant allele and he will develop the illness.
Since a male receives his single X-chromosome from his mother, the son of a healthy female silently carrying the deficient gene will have a 50% chance of inheriting that gene from her and with it the disease; and if his mother is affected with haemophilia, he will have a 100% chance of being a haemophiliac. In contrast, for a female to inherit the disease, she must receive two deficient X-chromosomes, one from her mother and the other from her father (who must therefore be a haemophiliac himself). Hence haemophilia is far more common among males than females. However it is possible for female carriers to become mild haemophiliacs due to lyonisation of the X chromosomes. Haemophiliac daughters are more common than they once were, as improved treatments for the disease have allowed more haemophiliac males to survive to adulthood and become parents. Adult females may experience menorrhagia (heavy periods) due to the bleeding tendency.
As with all genetics disorders, it is of course also possible for a human to acquire it spontaneously ( de novo), rather than inheriting it, because of a new mutation in one of their parents' gametes. Spontaneous mutations account for about ⅓ of all hemophilia A and 1/5 of all hemophilia B cases. Genetic testing and genetic counseling is recommended for families with hemophilia. Prenatal testing, such as amniocentesis, is available to pregnant women who may be carriers of the condition.
Probability
If a female gives birth to a haemophiliac child, she is a carrier for the disease. Until modern direct DNA testing, however, it was impossible to determine if a female with only healthy children was a carrier or not. Generally, the more healthy sons she bore, the higher the probability that she was not a carrier.
It is estimated that about 0.006% of the United States population suffers from haemophilia .
Treatment
Though there is no cure for haemophilia, it can be controlled with regular injections of the deficient clotting factor, i.e. factor VIII in haemophilia A or factor IX in haemophilia B. Some haemophiliacs develop antibodies (inhibitors) against the replacement factors given to them, so the amount of the factor has to be increased or non-human replacement products must be given, such as porcine factor VIII.
If a patient becomes refractory to replacement coagulation factor as a result of circulating inhibitors, this may be overcome with recombinant human factor VII (NovoSeven®), which is registered for this indication in many countries.
In western countries, common standards of care fall into one of two categories: prophylaxis or on-demand. Prophylaxis involves the infusion of clotting factor on a regular schedule in order to keep clotting levels sufficiently high to prevent spontaneous bleeding episodes. On-demand treatment involves treating bleeding episodes once they arise.
As a direct result of the contamination of the blood supply in the late 1970's and early/mid 1980's with viruses such as Hepatitis and HIV, new methods were developed in the production of clotting factor products. The initial response was to heat treat ( pasteurize) plasma-derived factor concentrate, followed by the development of monoclonal factor concentrates which use a combination of heat treatment and affinity chromatography to inactivate any viral agents in the pooled plasma from which the factor concentrate is derived.
Since 1992, recombinant factor products (which are cultured in Chinese hamster ovary ( CHO) tissue culture cells and involve little, if any human plasma products) have become available and are widely used in wealthier western countries. While recombinant clotting factor products offer higher purity and safety, they are, like concentrate, extremely expensive, and not generally available in the developing world. In many cases, factor products of any sort are difficult to obtain in developing countries.